Twin to Twin Transfusion Syndrome Stories
Read our Twin to Twin Transfusion Syndrome stories and learn about how other families have dealt with the condition. We’ll continually publish new Twin to Twin Transfusion Syndrome stories stories here. Only monochorionic twins can get Twin to Twin Transfusion Syndrome (TTTS). Monochorionic twins are twins that share a placenta. Only identical twins can be monochorionic. It’s important that you learn whether or not your twins share a placenta early on, so your doctors can know whether or not to look out for TTTS. Read more about determining chorionicity in twins.
Laura’s Twin to Twin Transfusion Syndrome Story
Mother: Laura Meyer (U.S).
Children: An older son and twin boys

When did you find out that you were pregnant with twins? What was your reaction?
“We found out we were pregnant with twins at our 10 week ultrasound. My husband and I were both shocked. We had been trying to get pregnant for nearly a year and a half, so for it to be twins was a little overwhelming. At that point we didn’t realize how high risk the pregnancy would be. But my OB immediately referred us to a Maternal Fetal Medicine (MFM) specialist because she knew the risk factors. At our first MFM appointment, we learned about TTTS and hoped it wouldn’t happen to us. Unfortunately, we became part of the 15 percent of mo-di pregnancies affected by TTTS.”
When did you find out that there were issues in relation to TTTS? What steps were taken?
“It was our 20 week growth scan. The ultrasound technician became kind of quiet as our scan went on. Shortly after he left the room, the doctor and our case nurse came in and broke the news. It was shortly before 4 central time. We began discussing where they were going to refer us to for complete diagnosis, consult and if necessary ablation. I remember being in shock, and the MFM was saying, not to pressure you, but if you want to be referred to Cincinnati, it’s almost 5 there, so we need to call them now before the office closes for the day. So we had to decide in about three minutes where we would have our full consult and possible surgery done. Our ultrasound was on a Monday, and we were in Cincinnati for tests and consult Thursday and had ablation Friday morning. During surgery they cauterized 33 connections in the placenta and drained 2.3 liter of fluid off of our recipient baby. It went so fast, but considering how fast TTTS could change, it was the best possible arrangement given our circumstances.”
How did the TTTS diagnosis affect you and your family?
“The diagnosis was difficult for us, since we had tried for a while to become pregnant. It was almost numbing to think about losing one or possibly both children that we had wanted for so long. Beyond that, we had so many things to arrange to be taken care of prior to leaving for Cincinnati. Our oldest at the time was 3 and about to turn 4, so we had to arrange for family to watch him, as we knew he couldn’t be cooped up all that time in a hospital or hotel for all the tests, surgery and time before follow up appointments. We also have a small farm with a flock of sheep, so we had to arrange for the sheep to be taken care of also. My husband and I also work full time, but thankfully both of our employers were super understanding of the situation. It was also difficult for me to limit my physical activity post surgery, as I’m so accustomed to being active and on the go.”
What was most challenging during it all?
“One of the worst parts of the whole thing was having to postpone our son’s birthday party until we came home. He turned 4 while we were away in Cincinnati for surgery. Following surgery, we had weekly ultrasound appointments. Again, my employer was super understanding of the situation and didn’t question the need for so many appointments. Thankfully our doppler numbers always looked good with one exception. There was just one week where we did have two ultrasounds two days apart, but thankfully it was a blip and they went back to normal range at the second appointment. I think that’s the hardest thing overall. The waiting between appointments and praying everything is okay.”
How did you cope?
“We had amazing support from our family and close friends throughout our journey. It was crucial to have shoulders to lean on or cry on if necessary. Without our family and friends, we might have gone completely crazy.”
When and how did you give birth?
“I went into labor at 30+6 weeks due to placental abruption.* It was exactly 10 weeks to the day I had surgery. I had my ultrasound earlier that week, and there were no signs at all that I would go into preterm labor. My cervix was closed and long, everything looked good. I woke up that morning and felt off. I had the day off, and called my husband at work and told him I had called triage and we’d go in so I could be checked. We drove 45 minutes to the hospital, and I was actually in labor at that time. I apparently have a pretty high pain tolerance, because I had felt no pain up until after we arrived at the hospital. The doctors attempted to slow things down, to buy some time for the steroid shot to work, but they wouldn’t slow down. I didn’t even have time for an epidural. I had arrived at the hospital shortly before 11 am, and the boys were born at 2:59 pm and 3:02 pm, both weighing 3lbs, 2oz (1417 grams). Both were born vaginally and head first. Our baby B had been transverse and turned head down after I had delivered Baby A.”
*Placental abruption is the separation of the placenta from the uterine lining.
How were your babies doing?
“At the time of our surgery, our donor baby was 20 percent smaller. So we were happy to have our donor make so much progress in a short time. But because we didn’t have the steroid shots, our boys had some extended NICU stays. Our recipient baby had a 38 day stay, while our donor had a 58 day stay. The Patent Ductus Arteriosus (PDA)* of our donor baby wouldn’t close on its own, so he had to have surgery. Our recipient was home prior to our scheduled induction date, and our donor was home before our due date, and both were over 6lbs (2721 grams) prior to discharge. Our NICU team would regularly comment on how they would never know that the boys were affected by TTTS if it wasn’t in their chart.”
*PDA is a condition wherein the ductus arteriosus fails to close after birth. PDA is common in newborns with persistent respiratory problems such as hypoxia, and has a high occurrence in premature newborns.
How are your boys doing at this point?
“Wonderful! Amazing! I just could go on and on about how miraculous they are. They are both over 25lbs (11339 grams) at 17 months of age, putting them in the upper half of the growth curve for actual age. They hit their milestones at their adjusted age or shortly before, with the exception of walking, and that was at 14 months adjusted age. To come to this point of having such healthy, active and bright boys after the fear of losing one or both of them because of TTTS can be emotionally overwhelming at times. We were beyond blessed to have such wonderful care throughout our whole journey. The speedy reaction to our diagnosis and our wonderful NICU team have given our boys the best outcome possible.”
If you were to offer some advice to parents in a similar situation what would that be?
“You do need to know enough about TTTS so you are able to advocate for yourself and your babies for the best possible outcome if that need arises. However, “Dr Google” is great at creating more fear and worry. So you have to walk the fine line between being informed and knowing so much your are scared out of your mind. Our whole pregnancy we had the best care possible, which I think was so important to where we at today. After our 10 week ultrasound, my OB immediately referred us to a MFM. At the first sign of TTTS, the MFM immediately sent us to Cincinnati. I know not everyone is so lucky. Time is of the essence with TTTS, and you need to act quickly if the situation arises. So if you are concerned, don’t be afraid to speak up, advocate or ask for a second opinion.”
Sign up for our newsletter or follow our Facebook page to stay updated on new TTTS or TAPS stories.




Leah’s Twin to Twin Transfusion Syndrome Story
Mother: Leah Kielt (Canada)
Children: An older son and twin boys

When did you find out that you were pregnant with twins? What was your reaction?
“I had my first ultrasound at 6 weeks. I had some bleeding and was worried, I was losing the baby, so I went to the emergency room. They completed the ultrasound and saw that there was a fetal pole and assured me the baby was okay. They then set up a second ultrasound in two weeks time to check on the baby again. I went back two weeks later and there was two of them! We were in so much shock, this pregnancy was not planned and then to find out there was two, it was a miracle.”
When did you find out that there were issues in relation to TTTS?
“I was seeing my Maternal Fetal Medicine (MFM) specialist at McMaster Children’s Hospital for ultrasounds. I remember this day like it was yesterday. It was the Thursday before Father’s Day weekend. At my appointment they expressed concern of increased fluid for baby b and a decrease in baby a. They made a follow up appointment for that Monday after Father’s Day. I was worried sick all weekend. I went back on the Monday and baby a now had no visible bladder and was wrapped in what they called saran wrap.*”
*When a baby has an abnormally low level of amniotic fluid, the membrane can cover the baby’s body, almost as if he or she was wrapped in saran wrap. It’s also sometimes referred to as being “stuck.”
What steps were taken?
“They called Toronto and told me to expect their call for an appointment. They gave me a note writing me off work. I went into my employer, handed in my note, and I was saying goodbye to my coworkers. As I am at work, I get the call from Toronto instructing me to come in tomorrow (Tuesday) for an 8am consultation. When I got to Toronto, I was 17 weeks pregnant and at stage two.* I thought at the time it was just a consultation, but they started asking for my insurance information during my consultation, and I knew at that point my babies were in danger, and I wouldn’t be leaving without the surgery. I was told that at stage two, the chances for both twins to survive was only 68 percent. I know that those are “decent” odds, but when it comes to the life of your babies, it’s not the odds you want to hear.”
*Read about the 5 stages of TTTS
How was the surgery?
“My spouse came to Toronto to be with me, so did my mother and mother in law. The surgery was a success. The next day they checked them on ultrasound and they found a bladder on my donor and his fluid was filling back up. It is truly amazing what the doctors are capable of doing. I’m very thankful to Dr Ryan and his team from Mount Sinai Hospital for everything they did for my boys and our family.”
How did the diagnosis affect you and your family?
“It was a very hard time. I still struggle with it daily – all the “what ifs.” I often wonder if I struggle from PTSD. It was a very traumatic time. I had a four year old at home at the time. Being over an hour away from him was hard, he didn’t understand what was going on. It was hard not having my spouse there for me as these are his first children. He had to return to work before I had the surgery. I am so lucky that I did have the support of my mother (who was in the operating room) with me and stayed the entire four days, I was there, and my mother in law who brought my oldest to visit. Everyday I am reminded how blessed I am to have two healthy 18 month olds – especially being on a lot of these twins Facebook forums where the outcomes aren’t always as positive as ours.”
When and how did you give birth?
“I gave birth at 33 weeks. On top of TTTS surgery I had high blood pressure, gestational diabetes and low iron. I was induced because of my high blood pressure. The boys were in the Neonatal Intensive Care Unit (NICU) for five days and then went to a step down hospital for three weeks to a special care nursery. Overall they did very well considering. Baby a was 4.3 lbs (1900 grams), and baby b was 4.6 lbs (1984 grams).”
How are your babies doing at this point?
“Excellent! Thriving very busy almost 19 month olds!”
If you were to offer some advice to parents in a similar situation what would that be?
“I think for me, I always had a positive outlook. Things went very quickly in my case, so I didn’t have much time to get upset about the situation. I put my trust in the doctors, and believed they would do what they could to save my babies. Everything happens for a reason, and if I was meant to be a mom to both of these babies it would happen. Also, I think something key is to educate yourself as soon as you find out you are having mo/di twins and to be aware of the risks, with information from a MFM specialist and to push to be seen by the proper medical team.”
Sign up for our newsletter or follow our Facebook page to stay updated on new Twin to Twin Transfusion Syndrome stories.


Elizabeth’s Twin to Twin Transfusion Syndrome Story
Mother: Elizabeth Hubartt (U.S.)
Children: Two older girls and twin boys

When did you find out that you were pregnant with twins?
“I found out, I was having twins, at my first obstetrician appointment at 12 weeks. The pregnancy itself was a surprise, so finding out they were twins was super shocking.”
When did you learn that there were issues in relation to TTTS?
“I found out I had TTTS at my second maternal-fetal medicine appointment during week 16. I was with my two girls who were 4 and 8 years old. They were excited to have baby brothers and it was the first week of summer break, so I thought the ultrasound would be cool for them to see. I immediately knew something was wrong based on the technician getting the more experienced technician, then getting the doctor. But she had shown me both heartbeats so I didn’t know what was wrong. The doctor came in and told me. I was really upset and scared, but tried to keep it together because my girls were there, and they could tell something was wrong, but I didn’t want them to be upset.”
What steps were taken?
“I was sent home and waited for the doctor to be in touch with dr. Ramen H. Chmait in LA. She called me back the next morning and our plan from him was for me to be monitored over the next several days, and as soon as it got worse, I would be sent to LA for laser surgery.
I went to LA for surgery about five days later and had surgery with dr. Chmait. I had stage 3 TTTS at that point. I met with a cardiologist as our recipient twin had moderate heart issues. I stayed overnight. I met with dr. Chmait and his team the next day and was then sent home. He advised my maternal-fetal medicine specialist for my follow up care from there.”
How did the TTTS diagnosis affect you and your family?
“My family was affected a lot. We were planning to move, and I was on bedrest. My girls were on summer break and both celebrated their birthdays a couple of weeks later. My mom and dad really had to help out a lot and my sister. She’s a teacher and was on summer break, so she was able to help. It was hard on me, I felt I had to stay positive for everyone and not to upset my girls.”
When and how did you give birth?
“I was induced at 36+0 weeks after my maternal-fetal medicine appointment the day before showed signs of growth restriction in twin A. I delivered both vaginally at the hospital in the operating room with epidural. Babies were both overall great. No NICU time. They ended up being 4lbs,5oz (1956 grams) and 4lbs,9oz (2069 grams). The bigger baby, twin B, had been estimated at 5lbs,3oz (2352 grams), so that’s why they thought baby A wasn’t growing. Twin A had low blood sugar, and they both had low body temperatures. After birth, twin A – who had the heart problems caused by TTTS – was signed off by a cardiologist. His heart had enough time to heal itself after the laser surgery, and no intervention was needed.”
What happened at the hospital?
“NICU nurses came to my room to monitor the babies. We had lots of skin to skin contact. The babies also had a little trouble eating, but did well enough – we went home after two days. We followed up with a pediatrician the next morning and then twice per week for two weeks to make sure they were eating and growing well. We had a follow up hearing test at the hospital for twin B because he failed twice in the hospital. He passed the third time.”
How are your babies doing at this point?
“At this point they are two years old and doing pretty well. They are meeting all of their milestones, if just a bit behind, but nothing worrisome. Twin A has non breathing episodes where he involuntarily stops breathing, if he gets upset or startled. We’ve seen a neurologist and cardiologist to rule anything serious out. He is fine overall and will grow out of these episodes, so we are told. They are scary.”
If you were to offer some advice to parents in a similar situation what would that be?
“Advocate for yourself and for your babies. I’m lucky my doctor was knowledgeable and sent me to dr. Chmait. I see many moms in my twin group that are not getting the best medical care, primarily because their doctors don’t know enough about TTTS and how it should be treated. Also, it’s okay to feel sad and nervous and anxious and worried. It is scary. I felt all of these emotions and then some.”
Sign up for our newsletter or follow our Facebook page to stay updated on new Twin to Twin Transfusion Syndrome stories.



Sarah’s Twin to Twin Transfusion Syndrome Story
Mother: Sarah Luter (UK)
Children: Big sister Kira and twin girls Erin and Cody

How far along were you when you were diagnosed with TTTS?
“I didn’t know that my twin girls had TTTS* until they were born so I guess my story will be quite different to other people’s. Firstly, after being told that I was unlikely to deliver two live babies after the complications with my singleton pregnancy 15 months earlier, I was absolutely delighted to have two babies, and so that was my focus. I was told that if I went into labour before 34 weeks they were unlikely to both survive. My eldest daughter did not develop well and was very unwell when she was born, hence the speculation that two babies would have less chance. Luckily I wasn’t as pessimistic and took comfort from my health, growing bump and positive scan results.”
*At about-twins.com we’ve asked Sarah if there’s a possibility that she could have had Twin Anemia Polycythemia Sequence (TAPS) as we think her story could indicate that. She had never heard about TAPS, the doctors told her TTTS. However, please note that TAPS is a recently discovered disease and this may be why she wasn’t diagnosed with it.
What was most challenging during it all? How did you cope?
“The pregnancy was only challenging for me emotionally when I needed to cope with other people trying to make me face what might have been an unthinkable outcome. I must also admit that at 22 weeks I had decided I wasn’t at all sure if I could cope with twins when my eldest was not letting me have any sleep.”
When and how did you deliver?
“I went into labour at 34+0 weeks. Cody was born vaginally not breathing and was resuscitated. She weighed 4lb, 4oz (1927 grams). Erin was nine minutes behind her sister screaming. She weighed 4lb,10oz (2097 grams). They were taken away pretty quickly and I only remember being surprised by how much hair they had – their sister was still bald at 15 months. When I had given birth the doctor who resuscitated Cody came to me and said ‘my wife is 16 weeks pregnant with twins, if she does half as well as you I will be very proud.’ I can’t say that out loud, it makes me cry, but that kept me going. Erin was in hospital for a check up 16 months later and that same doctor treated her – his twins were both doing well.”
When did you find out that they had TTTS?
“When we visited them a couple of hours later in the baby unit it was obvious how different in colour they were. Cody was very pale and Erin very red. The doctor explained the following day that they had a rare condition and that Cody may need a blood transfusion. However she recovered on her own remaining paler than Erin for a few months. And so I didn’t even realise how rare the condition was or what it meant until they were home and healthy.”
Did the news about TTTS affect you in any way?
“I do think I found the bright red twin less ‘cute’ so I dressed her in prettier clothes – that’s mad, I know that, and I’ve never shared it before. I have nightmares about Cody dying all the time but never the other two so maybe I see her as a weaker twin? Premature birth was the most horrendous thing to go through and I felt no one understood. I wanted to take my babies home and have that welcome home with my babies – I had to wait four weeks but they still went home. I sobbed like a child for most of the four weeks as I had when my first daughter was born prematurely.”
How are your twins doing today?
“Both girls are doing really well. They are 15 years old, they study hard, have had no serious health issues. Cody had a malformed front tooth which has led to years of treatment and she will continue to have until she is 21. Both girls compete in league trampolining competitions at national level.”
Sign up for our newsletter or follow our Facebook page to stay updated on new TTTS or TAPS stories.



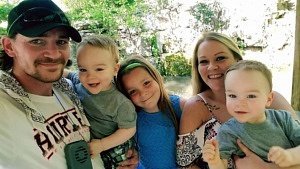
Renee’s Twin to Twin Transfusion Syndrome Story
Mother: Renee Cowley (U.S.)
Children: An older daughter and identical twin boys

When did you find out that you were pregnant?
“I found out I was pregnant very early on, at about 3-4 weeks. I was told by several people about this amazing obstetrician (OB) that was just 20 minutes from me so I made an appointment immediately. When I met him, it ended up just being a consultation and I didn’t get to see or hear the baby so I was pretty disappointed. My next appointment, I was about 10 weeks pregnant. He had an old ultrasound machine in the room I was in, so he was going to let us see the baby! We were so excited. Jon, the children’s father and my boyfriend of 13 years, was there with me. As the doctor is moving the wand around showing us different things, he says “There are two!” To which, I responded “Two what?!?!?” “Two babies!” he said. He told us he would give us a minute to process the news which happened to be the exact moment I lost it. I started crying and was scared to death. TWO BABIES?! HOW? ME?? IS THIS A JOKE?! Jon paced the floor back and forth and promised “it’ll be ok.” I went home and started researching everything “twins” possible. It started sinking in that I was having TWO babies and mom, dad and big sister all got very excited!!”
When did you get to see your babies again?
“Finally at 18+4 weeks, we had our first “formal” ultrasound on a real up to date machine. We found out we were having two boys and we were so very excited. During the ultrasound, they were unable to find a dividing membrane and diagnosed us as having monoamniotic-monochorionic twins aka mo-mo twins. We also had the quad marker test done this day. The doctor explained that we would still be seen every four weeks until 30 weeks when we would be seen every two weeks. Delivery would be as close to full term or 40 weeks as my body would allow, he said. We would not be referred to a MFM (Maternal-Fetal Medicine) physician unless “things get out of my control,” he said. This is when I started to feel really uneasy about my decision. I had already learned from the Modi Pregnancy page on Facebook that I should be seen every two weeks from 16 weeks by a MFM who does all the proper doppler scans and that 40 weeks was absurd.”
When did you see your doctor again?
“The doctor went on vacation at this point and failed to mention that he would not be in the office for 11 days. I called to get the results of the quad marker screen and to inquire about the ultrasound. I was told that he was out and I would have to wait for his return. There was not another doctor that I could discuss this with and if I had an emergency to call 911 or go to the emergency room. Halfway through his vacation, for some reason, I became very anxious and kept getting the feeling something was just “off.” I was super tired – more so than normal – my stomach felt bigger and harder than it had been and it was harder to breathe. Friends and family thought maybe I just researched too much and scared myself. Looking back, I think it was mother’s intuition the whole time. 11 days passed and I waited half of the day for the doctor to call. Finally, I called him and was told that he would be referring me to a MFM physician because we had a 1/65 chance that the babies had Downs syndrome with screen testing positive and that we had developed polyhydramnios.”
What happened after your referral?
“On Wednesday April 29, 2015, at 19+4 weeks, we were sent almost two hours away where they confirmed that we were showing signs of TTTS and that baby B had no bladder. He explained TTTS to us and told us that he was referring us to KU Medical Center, to one of the few doctors in the world who could perform the laser ablation surgery needed to correct the issue IF it progressed any further. Without that referral we would have had to travel 650 miles to Cincinnati or 1900 miles to Seattle – whichever one felt that they could help us best. I got into the Center for Advanced Fetal Care at KU Medical Center the same day and met with Dr. Carl Weiner. We had an ultrasound done there, where they finally discovered a dividing membrane. This was great news and we were now told we were having monochorionic diamniotic twins aka mo-di twins. Although they did also confirm that we were borderline TTTS* and would need to come back in a few days to keep a very close eye on it.”
* Twin B had a 2.6 x 4.2 cm pocket and no bladder was seen. Twin A’s deepest vertical pocket of fluid was 7.85 cm.
How were you feeling?
“I was terrified. I was shocked at first of the thought of two babies, but that fear turned to love and I was supposed to have TWO babies now. Everything was supposed to be ok with BOTH of them. TTTS only affects like 15 percent of twin pregnancies so there was “no way it would be us,” I thought. But, I had already read so much on this subject that I had a good idea of what we were up against. Jon was terrified as well but he stayed strong for both of us. He had me relax while he took care of everything that we needed done. I went back to KU for a follow up ultrasound two days later. My fears were coming true. We had progressed to Stage 2 TTTS* and were told surgery was highly recommended. We then scheduled the laser ablation surgery for the very next morning. He also planned on removing the excess fluid and would test it to further explore the possibilities of the babies having Downs syndrome.”
* Twin B had no fluid at all and Twin A deepest vertical pocket was 10.25 cm.
How was the day of your surgery?
“The next morning we arrived at the hospital with a few close family members. I was 20+0 weeks exactly. Doctor Weiner came in and explained the process, pros, cons and risks to all of us. We had another ultrasound done to confirm surgery was still needed. I didn’t think to ask what stage we were at this point because we were stage 2 TTTS just the day before. My discharge papers from the NICU showed stage 2, but as I am gathering information for this interview, I call my favorite nurse to find out our exact fluid measurements and stage of TTTS and almost two full years later I find out my boys had stage 3 TTTS, not stage 2!!! The discharge paperwork had a typo. This means I went from borderline TTTS to Stage 3 in only four days.”
How were your babies doing?
“Baby A was developing hydrops and baby B had an abnormally elevated MCA doppler & reversed ductus flow. Additionally, baby A now had 11.5 centimeter of fluid measuring the deepest vertical pocket and Baby B had zero. He was “stuck” and had no fluid, no nutrients, no bladder. Baby A “the recipient” was at risk of heart failure as the overflow from Baby B “the donor baby” was rushing him and baby B was not getting the things he needed to survive. We were told that surgery was risky but that without surgery we only had a 20 percent chance that either of the babies would make it. With surgery, we were told we had a 70 percent chance that at least one baby would survive and a 30 percent chance that both would survive. I had an anterior placenta so they feared this would complicate surgery even further.”
How were you doing at this point?
“I had to sign all these different forms stating I understood the risks. The hardest part of that was signing a piece of paper that stated if my doctor could not successfully complete the surgery we would allow him to tie an umbilical cord off to save at least one of the babies. They would save whoever had a better chance of survival. That is something no mother should ever have to consider but was something I had to do in order to save one of their lives if surgery was unsuccessful. I had some time with my family before surgery. Then the nurses came in and said it was time.”
How did the surgery go?
“I walked to the operating room with just a few nurses and found about 20 more staff waiting. I climbed up on the operating table, talked to the anesthesiologist for a minute, said one plea to God and was out. I woke up what seemed to be 10 minutes later in recovery with a bunch of strange faces standing around and Jon beside me. I hear Dr. Weiner say “they both look great.” I have never been so overwhelmed with happiness in my life. Both my boys made it through surgery. Although we weren’t out of the woods yet, he explained. The surgery is very stressful to the babies. He had to laser 19 connections and remove four liters of excess fluid around baby A. He said he had never seen so many connections before like that, but the surgery went so much better than he expected and they would just keep a very close eye on things.”
How did you feel?
“Physically, the surgery wasn’t painful at all. The worst part physically was a stiff neck because of the position they had to put me in to reach the placenta and a sore throat from the breathing tube. I only had a tiny little incision on my side. I stayed overnight and had an ultrasound done the next morning. Dopplers were evening out and baby B had a visible bladder again. This was great news and I was released later that day with orders to come back once a week for additional monitoring. Because of the surgery, we would now set our induction date at 34 weeks. That also meant four hours of driving once a week for hopefully 14 weeks for MFM physician appointments and biweekly visits to the OB. But knowing my boys were ok, made it 1000 percent worth every minute of driving.”
What about the possibility of Downs syndrome?
“During this time, we also found out from the amniocentesis performed during surgery, that our boys did not have Downs syndrome. More great news. Twins are apparently harder to test for with the quad marker screening test and usually show to be more at risk. We had precautionary steroid shots given at 24 weeks and my “donor” baby aka the small baby was now my “big” baby. Something about the surgery caused them to switch but other than that things were progressing great. From there on, each appointment went pretty well. Normal dopplers and growth. I started my first day of maternity leave finally on July 22, 2015.
I had my 32 week appointment the following day. I figured that I would have two weeks to relax and finish getting ready for the babies and our big move. Yes, we bought our first home and were closing at the same time they were due! Go big or go home right?”
How did your 32 week appointment go?
“It was a pretty normal appointment at the beginning and then I noticed the ultrasound technician appeared to see something wrong or off as she kept trying to get a “good measurement.” It turned out that baby B was showing elevated ductus dopplers. I was admitted to the hospital and Dr. Weiner explained that he suspected that they were developing TAPS. At this point, he said that the babies would be “safer out than in” and the plan was to start the second round of steroids. I would get one shot that day, another 24 hours later and then we would begin induction 24 hours after that.”
How did the induction proceed?
“The plan went accordingly and we began the induction process Friday night at 6pm by using a transcervical foley balloon. This was so painful. After a few failed attempts, the nurses said that the epidural was needed to get the balloon into place. With the epidural going and the labor process beginning, I tried to rest as much as possible. The next day, I had Pitocin* and my family visited. I continued to rest as things moved rather slowly at first. Because I had to get the epidural early, the entire labor process was really not that bad pain-wise. I was dilating about one centimeter an hour. 3pm – 4cm, 4pm – 5cm, 5pm – 6cm. I started feeling very nauseous and ending up getting sick. The nurse came in and checked me right after stating that is often a sign that you “are ready.” Sure enough, I was at a 10 cm. and she said “it’s time to go.” All of a sudden, I wasn’t ready. We were supposed to be at a 7 cm. – not a 10. I was wheeled to the operating room so that if anything unexpected happened, they could perform an emergency c-section. I began pushing at about 5:50 pm. At 6:02 pm, Baby A, Matthew Isaac was born. He came out with the cord around his neck, but crying. Eight minutes and just a few pushes later, Baby B, Malachi Allen was born.”
*An induction with Pitocin means your doctor or midwife will induce your labor using a medicine called Pitocin, which is a synthetic version of oxytocin.
What were your thoughts on giving birth vaginally?
“Dr. Weiner actually encouraged me to try. I asked for a c-section date and about hit the floor when he said that wasn’t necessary. I had my daughter in 2008 and after 51 hours of labor and 2 1/2 hours of pushing, I had to get a c-section for “arrest of descent.* I was actually more nervous about having a vaginal birth after c-section (vbac) than having a c-section, just because I hadn’t delivered that way before. But I am so thankful he talked me into it because it was the best experience of my life.”
* Failure of the baby to continue to descend during the second stage of labor despite contractions and pushing.
How big were the babies?
“Matthew weighed 3.6 lbs (1530 grams) and was 16.5 in (42 centimeters) long with apgar scores of 9 & 9. Malachi was born weighing 3.14 lbs (1757 grams) and was 16.1 in (41 centimetres) long with apgar scores of 8 & 8. He came out crying as well but did require CPAP for 24 hours followed by oxygen for another 24 hours. They were so tiny, but absolutely resilient. We spent 26 days in the NICU for anemia, temperature control, bradys*, and learning to feed and grow.”
* Bradycardia is the medical term for a heart rate that is too slow.
How were you feeling?
“I was two hours away from my family, I was discharged from the hospital and couldn’t just take my babies with me. Needless to say the pregnancy and birth was very hard emotionally. The NICU thankfully had a pull out couch and I was allowed to stay there the entire time though. We had a few visitors and daddy and big sister came to visit often but it was mostly mommy and babies learning as much as we could from all the wonderful doctors and nurses while we were there. Matthew & Malachi were finally released weighing 4.2 lbs (1871 grams) and 4.9 lbs (2069 grams) and feeding like champs every three hours at 26 days old.”
How did your daughter respond to her brothers?
“Big sister McKayla was absolutely in love with them the moment she saw them. She was an only child for seven years so she was ecstatic when she found out she was going to be a big sister. She actually predicted I was having twins before we even knew. Now that the boys are almost two years old, she is always loving on them, reading to them, chasing them, and playing with them. She is also a huge help whenever needed. We couldn’t have asked for a better big sister for them.”
How are your sons doing now?
“Matthew and Malachi will turn two in just a couple of months! Time is flying and it doesn’t even seem possible. They are learning so much everyday. They were walking at one year, speaking about 20 words at 18 months, and are getting into absolutely everything they can. They are sooo fast. They love to dance and play with blocks and books. They are so silly and love each other so much as well as the rest of their family. Watching them grow has been an exhausting blessing and I wouldn’t change it for the world. At their 18 month appointment they were in the 99th percentile weighing 28 lbs (12.7 kilos) and 30 lbs (13.6 kilos). They are big healthy boys now and you’d never know they were two months premature.”
If you were to offer some advice to parents in a similar situation what would that be?
“My advice to any parents expecting identical twins would be to research. Research everything. Proper mo-di care guidelines. TTTS. Delivery timing of mo-di twins. Make sure you get an OB who really understands mo-di twins. Also make sure to have a MFM physician and that you are seen biweekly from 16 weeks on with all the proper scans. If you are NOT receiving that care, FIGHT for those things. We are the only advocates our babies have. There are far too many OBs who do not know the proper mo-di care guidelines and we lose far too many babies a year because of this. TTTS has no specific cause. It is not something you did, or can prevent. It comes out of nowhere and can progress VERY fast so being knowledgeable and fighting for proper care are the only things you as mom, can really do.”
Sign up for our newsletter or follow our Facebook page to stay updated on new Twin to Twin Transfusion Syndrome stories.



Kathleen’s Twin to Twin Transfusion Syndrome Story
Mother: Kathleen Smith Forbush (U.S)
Children: Triplets – identical twin boys and fraternal twin boy

When did you become aware that you were pregnant with triplets – and that you were having mo-di twins?
“We found out at our six week ultrasound. I did IVF but was given low odds of success so we transferred two embryos. The possibility of one splitting and ending up with triplets never crossed my mind. I had never heard of TTTS prior to getting pregnant.”
How far along were you when you were diagnosed with TTTS?
“I found out at an ultrasound at 23+1 weeks. We were having weekly ultrasounds at my request, not due to TTTS but because I was just worried in general. At our 21 week ultrasound everything including fluid levels looked great – although the weight discordance between the twins did increase – and our next appointment was set for two weeks instead of one.”
How did you become aware that something wasn’t quite right?
“My husband and I knew something was wrong when they did measurements and our baby B who was always slightly bigger had a large jump in size compared with the other two. When the ultrasound technician left and said she would be right back, we did not know what was going on but knew something was not right. Shortly afterwards the doctor came in and told us we had stage 4 TTTS and needed to get to Cincinnati as quickly as possible as we were in Nashville where there are no surgeons. My husband was very calm and began setting everything up. I was understandably upset and honestly a little bit in shock.”
What kind of treatment were you offered?
“The only treatment we were offered was laser surgery given we were stage 4 and things looked very dire. We were able to get to Cincinnati at about 5pm and went straight to the hospital where we met the doctor and had a very long in depth ultrasound. They debated doing the surgery that night but ultimately decided to start me on procardia to strengthen the boys hearts. I stayed on it the remainder of the pregnancy for that purpose. They had me come back the next morning for surgery if the babies survived the night. That night was possibly the longest night of my life knowing I could do nothing and fully comprehending the seriousness of what was going on.”
What happened the next morning?
“Thankfully we had three heartbeats when we showed up the next morning. We met with the surgeon who went into more depth about what he would be doing and we met with a neonatologist as well. The neonatologist explained that with the babies being only 23+2 weeks and very sick, the odds were not good if I were to deliver. I remember crying a lot. I was given an epidural, local anesthetic and mild sedation. I don’t know if they always sedate people but I was extremely emotional so that might be why. I remember waking up during surgery for a brief time and they asked if I wanted more medicine and then waking up after surgery. I have read about people being awake the whole time but to be honest I’m glad I wasn’t. I don’t think I would have been calm. I didn’t sleep literally at all the night before.”
How did your children respond to the surgery?
“Our babies made it through surgery and we were told the next 24 hours were critical. I stayed overnight in the hospital and thankfully the boys had strong heartbeats the next day.
We were given a less than 10 percent chance of double – well in our case triple – survivors. One of the doctors in Cincinnati later told me that everyone on the team went into surgery expecting to, but obviously hoping not to, lose our recipient. They were amazed that throughout surgery his heart rate never dropped below 60 and at what a little fighter he was.”
What happened next?
“The next hurdle was them making it one week and adjusting to the treatment and recovering. Our recipient baby had been in congestive heart failure and had hydrops so they were particularly concerned about him. One week post op our donor looked great and our recipient was showing signs of improvement but his heart was still quite sick. We also did a post op MRI scan that week where we discovered that our recipient had suffered a brain bleed due to the distress he was under. I was devastated but the doctors were very compassionate, they were honest in telling us that he would be at high risk of complications such as delays after birth but there was no way to know. Our best hope would be that it resolved before birth. They also explained that babies’ brains are very plastic and can rewire around damage and recover sometimes with no lasting or serious effects unlike adults. From there we monitored his ventricles through ultrasounds and we were able to tell that it was not getting worse but not much more than that.”
Where did you stay?
“Because of the complications and our recipient baby’s heart being sick with the possibility of surgery needed depending on when I delivered, we decided to stay in Cincinnati and continue monitoring there as we wanted our TTTS surgeon to do the heart surgery if necessary. I was put on bed rest. I started out at bed rest at our temporary home and ended up inpatient at 27 weeks due to some signs of preeclampsia. At 30 weeks our recipients heart was healed to the point that doctors did not think he would need surgery after birth so we transferred back to Nashville and the care of my original Maternal-Fetal Medicine (MFM) physician. I went immediately back on hospital bed rest and delivered at 32+5 weeks.”
When and how were your babies delivered?
“My babies were delivered by c-section at 32+5 weeks on March 20, 2015. I was doing well, as were they, but I had started leaking fluid about three days prior and my doctor decided it was time to deliver. We had two sets of steroid shots, one at 27 weeks and another at 32 weeks. My donor was born first at 4lbs, 4oz (1927 grams), recipient second at 3lbs, 11oz (1672 grams), and my bystander last at 4lbs, 10oz (2097 grams). One baby needed no oxygen and the other two had room air nasal cannulas* on for a few hours. The boys all did really well in the NICU and were only there as feeders and growers for a little over two weeks. Our recipient had a cardiac echo which showed his heart had fully healed and a head ultrasound that showed that the bleed in his brain had completely resolved.”
*A nasal oxygen cannula is a piece of equipment that delivers additional oxygen or air flow to babies who need help breathing.
How are your boys doing now?
“The boys are a little over two years old now and all doing great. My recipient has some minor optical issues but he wears glasses and we patch for that. Physically and cognitively he is on track as are his brothers. We are very lucky.”
What was most challenging during it all?
“There were several challenges but I think the biggest one was just having no control over the situation. I went from a relatively easy multiples pregnancy to being rushed to emergency surgery in a matter of hours.”
Is there anything you wish you had done differently during it all?
“I still struggle with the what ifs, such as what if we had gone in weekly as we usually did? Would they have caught it, or on the other end of the spectrum, what if we had gone in at 22 weeks and decided to push to every two weeks then? I know my boys would not be here had that been the case. My doctors believe our TTTS came on very suddenly in a matter of days and looking back I recall my belly feeling very tight and being very uncomfortable starting about 3-4 days before the diagnosis. Unfortunately I had no clue those could be warning signs of TTTS. I had a wonderful MFM physician who did tell us a little about TTTS at our first appointment but if there is one thing I could change it would be giving patients more information about the disease and more monitoring.”
If you were to offer some advice to parents in a similar situation what would that be?
“My best advice for parents is to make sure they have a doctor who knows about TTTS and proper monitoring. In addition do your own research, join support groups, and trust your gut. I wish I had done more of all three of those things.”
Sign up for our newsletter or follow our Facebook page to stay updated on new TTTS or TAPS stories.



Stephanie’s Twin to Twin Transfusion Syndrome Story
Mother: Stephanie Ernst (Australian, living in the Netherlands)
Children: Twin girls Emilie and Mathilde

How did you find out you were pregnant with twins?
“My story starts in early June, 2013. In 2012, we lost our first baby at 9 weeks in a miscarriage, so to say that this pregnancy was both welcomed and feared is not an understatement. At 7 weeks, we met our little parasite – at this stage, singular parasite. The other was tucked away behind her sibling in a bizarre game of uterine hide and seek. We found it had a heartbeat and everything looked fine. I was then booked in for a 10 week dating scan. The technician probed and prodded for a few minutes, whilst I am silently waiting for the worst possible news … this pregnancy was also non-viable.”
“So, they told you you’re having a baby?”
Horrified, I answered “Yes, that’s right.”
“Ok, here it is. And here is the other.”
“Are you kidding me?” By this time, my husband Marius is laughing at me.
“No, I’m not joking”
“No way!”
“To be honest, anything after that point is a blur, although I do recall asking if I could have vodka. I was referred to the resident twin specialist in the hospital, and an appointment booked for the following week. Our meeting was interesting, with him explaining the risks associated with having monochironic twins, including a brief chat about this thing called ‘Twin To Twin Transfusion Syndrome’ which happens in some pregnancies. ‘But don’t worry!’ he said. ‘It’s really rare. You won’t get it.’ Yeah, right.”
How did you feel at the beginning of your pregnancy?
“Other than horrendous morning sickness to 18 weeks, and being diagnosed with a shortened cervix at 20 weeks, everything progressed really normally. The girls passed all their checks with flying colors. It was amusing to tell all our family and friends that yes, we were actually expecting two babies and it was amazing to make plans for their future.”
When were you diagnosed with TTTS?
“At 23 weeks, I went for a routine check-up like I had been every two weeks. On the ultrasound they discovered a massive discrepancy with amniotic fluid. The technician found out that twin A had a fluid pocket of 1.5 cm, whilst Twin B was 10.5 cm. Baby a had so little fluid she was ‘stuck’ to the wall of my uterus. I was in shock. The doctor immediately referred me to Leids Universiteit Medisch Centrum (LUMC) in Leiden, because they are leaders in TTTS research. I think both my husband and I were in shock at the seriousness of the diagnosis, and the speed at which things happened. I was diagnosed at 10am in Almere, by 1pm I was seeing doctors in Leiden.”
What happend at the hospital in Leiden?
“I will be honest here when I say that our first appointment is not the fondest memory of LUMC that we have. We’d rushed from Almere to Leiden, had multiple echoes and were now having our worst fears confirmed. We were given the choice to terminate the pregnancy, to participate in a trial for laser treatment, or to just ‘wait and see.’ We chose the wait and see option, based on the information at hand. The doctor raised the topic of the laser surgery trial, and we said we would discuss it. The doctor pressured us again, and this time after we stated that we would consider it if things got worse, we were told we should probably make funeral plans for our babies. We had been given a diagnosis that gave our little ones a death sentence. We were heartbroken to have come this far and be told that things were going to get worse. Naturally, we were shocked but I lodged a complaint and had excellent care after that. It was decided at the next appointment I had that we would monitor the situation carefully, and decide on surgery if the situation deteriorated. Thankfully, things stabilized and although they only improved slightly, the girls defied odds. My donor twin was amazing. She showed very little signs of stress and at every ultrasound had a very, very visible and full bladder she liked to empty on cue.”
How did the following weeks progress?
“To be honest, the next few days blurred into weeks. Our whole lives revolved around the hospital. I was there every three to four days for echoes, with that thought that something could go incredibly wrong. Thankfully, it seemed everything was ‘stable.’ I had conversations with a few different doctors and it seemed I was always given different information – sometimes conflicting. It wasn’t really until I talked to one doctor who took the time to explain about TTTS, and then also about this other strange thing – TAPS, which I was told may be developing because one twin was a little anemic. ‘But don’t worry,’ he said. ‘That’s not really a big concern right now. We’ll just monitor it.’ Miraculously, the fluid levels began to equalise. Twin A grew a little slower than Twin B, but she was growing again. Other than the fluid levels – and with only a slight indication of anemia in twin A – things were progressing well. We were monitored every three days to start with, then went to weekly at 28 weeks.”
How were you feeling?
“The commute to the hospital was difficult, as it’s about an hour and a half from my house to Leiden, and being very heavily pregnant on public transport is awful.
I had it in my head that we only had to make it to 28 weeks. For some reason, this was the magical milestone. At 27 weeks, we were actually given clearance to go back to Almere hospital for alternating visits. Things were starting to get better and we really truly started to relax. We finished the baby room, and started to look forward to Christmas. It never really left our minds that at any stage this could all go downhill, but for the moment, things were good. Every appointment showed the same thing … ‘no change.’ They were also watching the anemia, which whilst it was there, really didn’t change that much.
Then it came to December 10. I had my routine weekly appointment that day at 30+6 weeks. This time at LUMC.”
What happend that day?
“I’d gotten on the table as normal, and watched what was going on. It was taking much longer than normal – and when the echo technician left the room to consult with a colleague, I guessed something was wrong. Being a veteran – at this stage, of around 21 echoes – I could already see that something wasn’t quite right with the readings. I knew that the anemia had worsened. However, the technician was rather vague in his comments to me, and his colleague explained that the blood discrepancy between the girls had worsened. My dopplers had gone from being just out of the ordinary to off the charts. To top it all off, they believed they had seen a shadow on the brain of the recipient twin. It was time to make some serious decisions. I was told we could deliver, or terminate. I really, really hope that the termination reference was one of those ‘lost in translation’ things, as I’m an Australian living in the Netherlands. The decision was made to deliver ASAP via c-section.”
How did things progress?
“By now everything was a rush. I was admitted to the LUMC, given my first wonderful steroid injection at 2pm, and hooked up to have a couple of CGT’s. I called my husband, who then in turn called both our parents. He stopped at home and picked up my hospital bag, my laptop and my phone charger. I hadn’t completed packing it, to my horror I forgot all extra pairs of underpants and a hairbrush. We knew on the 12th of December that sometime before 2pm I’d have the C-section. My girls would be delivered at 31+1 weeks.”
How was the day of your c-section?
“We weren’t prepared for how fast it all happened. At 11am, my room filled with people, preparing us for theatre. I was then sent down to delivery. At 12.31pm Emilie was delivered. I didn’t hear a sound, and she was whisked away. At 12.33pm Mathilde was delivered. She screamed like a banshee. We had no idea what was going on. Next thing, a nurse came back with Emilie and I was introduced to my oldest daughter. To be honest, when I first saw her, I cried. A lot of emotions went through me. It was a fleeting visit, and she was whisked away again whilst I was sewn back together and my husband went with the girls to the NICU. I get stitched up, and taken to recovery. It was a couple of hours before I actually got to see the girls – Emilie, still tiny, skinny and white – and my first look at Mathilde, bloated and red, and both incredibly ugly. My donor – twin A – was 1106 grams (2lb, 7oz) at birth, my recipient twin 1590 grams (3lb, 8oz).”
What happend in the evening?
“I remember being in my hospital room, and smelling the food coming around. I had not eaten since the night before, so as you can imagine, with the stress of the day and the lack of food, I was starving. A man in hospital uniform walks into my room, carrying a covered tray, and automatically I assumed it was my dinner. As the table is pulled out, and the cover is lifted, I am greeted with … the placenta. It was dyed pretty colours – red and blue for Emilie, green and orange for Mathilde – but all my poor brain can process is ‘I thought this was my dinner.’ Dr. Lopriore, the man in the hospital uniform, was extremely enthusiastic and it was very interesting – but still – I don’t think I was quite prepared for that shock. He then asked if he could take it and do some further study on it. ‘It’s yours, really.’ I said. ‘No, you need to sign a paper,’ he said. ‘Do you have a pen?’ Anything really to get this off my table! I signed over my rights to the amazing technicolour placenta, and I could actually swear that once this was done, he raced out of the room with his ‘precioussssss.’ Needless to say, the poor guy who delivered my dinner shortly after that probably thought it was a bit unusual that I asked if this really was dinner time.”
How were the girls doing?
“The girls spent a grand total of 12 days in the LUMC NICU. On Christmas Eve, they were transferred to the Flevoziekenhuis in Almere, our local NICU. After five weeks, my recipient twin was deemed healthy enough to go home, and a week later, the donor (who mostly had weight issues) was also allowed to come home. Mathilde came home from hospital on January 16, weighing 2300 grams (5lb, 1oz), Emilie a week later on January 24 weighing 1900 grams (4lb, 3oz). Emilie is a veteran of three blood transfusions before she was a month old, Mathilde has had two blood extractions.”
How are your girls doing today?
“My girls are now healthy, active and extremely funny three year olds. They are very young for their age, and they do have some speech delays, but in general they are funny, smart and sometimes more than a bit cheeky. We are well monitored here by both our local hospital and also the LUMC – and will be until they are eight years old. It’s amazing how far they have come.”
How are you doing?
“Right now, I am doing well. It has taken three years to come to a point where I am able to hold in the emotions that come up when I talk about this. I spent time with a wonderful counsellor, who helped me no end. I still get very emotional when I see babies in incubators, and when I hear stories about TTTS, especially those about babies who don’t make it. That could have been me, if I didn’t have the amazing care that I had here in the Netherlands. I am very grateful to the staff of LUMC, in particular those who had anything to do with our case before, during and after the delivery.”
If you were to offer some advice to parents in a similar situation what would that be?
“If you ever find yourself in a situation like this – please, you are not alone. Find groups on Facebook, look on the internet for support groups for TTTS. The people there know what you’re going through. I thought I had to do it alone, and it’s only recently that I’ve found all these amazing groups who listen to you and take the time to reassure you.
Ask lots of questions, and challenge the doctors if you feel like they aren’t explaining things. If you’re doing things in a second language, like I was, ask for links or literature in your native language. They exist, and it will make your life so much easier.”
You were diagnosed and received treatment in a country where you barely spoke the language. How did that affect you?
“It was so hard. I could talk to my parents by phone, but it was still a time where I needed support and family by my side. I am thankful my husband’s family was here to give us love and help. I became very depressed though, and was seeing a counselor to help with all the overwhelming emotions. Not speaking Dutch was difficult. The medical staff were excellent, but there were a few times where things were lost in translation. Also, when it came to the possible TAPS diagnosis, there was so little information in English out there about it. Things are scary when the information you have is in another language, or not available.”
Is there anything you wish you’d done differently during it all?
“Tell people about what’s going on in your life. You’re going to be seeing a lot of doctors and medical staff – especially if you end up in the NICU. Get coffee, talk to people, try to escape the world of neonatology for at least an hour just so you feel normal. Make a list of the people who offer to help, and don’t be afraid to ask. During pregnancy, I honestly wish I hadn’t kept the difficulties and the problems we were having so ‘on the down low.’ Talking about it and letting people know why you’re not yourself is so much more honest, and whilst they may not understand, they should have some empathy towards your situation.”
Sign up for our newsletter or follow our Facebook page to stay updated on new Twin to Twin Transfusion Syndrome stories.






Laura’s Twin to Twin Transfusion Syndrome Story
Mother: Laura Russell (AU)
Children: Twin girls Daisy and Rosie.
Laura Russell is a member of a grief support group for double or single loss mums based out of the U.S. Read more about the TTTS grief support group.

When was TTTS detected?
“It was detected in week 33 with Daisy not growing anymore and the cord flow changes. My scans were never fun towards the end of my pregnancy. A couple of hours each time, numerous doctors, many opinions. In week 33 I had a troubling scan, my third scan that week. I was told after four hours of waiting and discussions with doctors that “these babies need to come out today.” I asked what the worst case scenario was if they didn’t, I was told “you don’t wanna know.” Nevertheless, they said that they could not admit me that day as unfortunately no bed was available, with two incubators, so I was sent home to return at 7 a.m. the next morning for my emergency c-section. I had a steroid injection and went home.”
How did you feel about needing a c-section?
“My mentality was “if I can do them no more good inside me, let’s get them out and fix them on the outside.” There was absolutely no room for guilt at not being able to carry them any longer, this was becoming a life or death situation. I always wanted a c-section as the other option terrified me! I have two bulging discs in my back so didn’t want to risk back injury from labour even before I found out it was twins. When I found out they were mono-di, the c-section was booked in for 36 weeks with three steroid injections booked the weeks before. In the end, we only had one the night before delivery.”
How was the day of your c-section?
“I turned up at the hospital 7 a.m. the next morning. I was admitted to a room and given a gown, I was ready to go. It was a Saturday, yet another change of staff, a new obstetrician introduced herself to me and informed me “we are going to postpone you till Monday, we don’t have enough staff and someone is coming in requiring brain surgery.” I said “NO! Absolutely not, if the doctor told me these babies need to come out yesterday then I need you to go away, call him, check my scan records, THEN come back and tell me what you’re going to do!” I didn’t even have the name of the doctor, but 15 minutes later the obstetrician came back to my room and informed me that they would be taking me down immediately.”
How was the delivery?
“Daisy was born at 1.06 p.m., Rosie followed six minutes later. Daisy was handed to my husband while they struggled to resuscitate Rosie. She was 1.5 kg (3lbs, 4oz). I look back now and I know this was a diversion. They knew TTTS had set in and they knew how sick Rosie was otherwise why would they hand us Daisy so quickly? The doctors stabilized her and wheeled her past us in an incubator saying “we need to get her upstairs now.” I said OK, I was fine, I have no other children so I had nothing to compare it to. My husband went with her. According to Rosie’s discharge notes they did 11 things to her in six minutes to stabilize her, she was intubated and placed on oxygen for 48 hours. I held her when she was three days old. When I was back in my room later, the obstetrician came and apologized to me, “we shouldn’t have put you through that” she said, “Twin to Twin Transfusion Syndrome is sometimes detectable, and can be treated with laser, sometimes not, at three scans a week in those last week’s still nothing showed up, it can set in during delivery.” Mine was just not found until week 33. Daisy had stopped growing and her cord blood flow was slowing down.”
How did the following months go?
“At eight months, at a routine maternal health check, the nurse thought Rosie’s head was growing too quickly. We took Rosie to the doctor and she agreed. We were referred to a neuro-surgeon. Rosie then underwent an MRI under sedation and the neuro-surgeon diagnosed her with hydrocephalus.*
Due to the ‘heroics’ the doctors put her through to save her life shortly after birth, we believe cranial bleedings were caused, these, as is very common in premature babies, went undetected. They in turn scarred over, blocking her ventricles in her brain. They operated to relieve the pressure and inserted a shunt. This will drain her brain fluid into her tummy for the rest of her life.”
*Hydrocephalus is a condition that occurs when fluid builds up in the skull and causes the brain to swell. The name means “water on the brain.”
How has this affected your family?
“My twins are TTTS survivors but its not been without anxiety, trauma, and now an ongoing illness. It requires my husband and I – and anyone in contact with Rosie – to be diligent with her care. If she vomits, has a continuing high temperature or becomes lethargic she needs to go to the emergency room. We’ve been admitted to hospital multiple times since her shunt was inserted at eight months old. At three years old her shunt began to malfunction almost weekly, I collated stats like a nurse over six months, tempature changes, how many times she vomited, did we go to hospital, yes, no. It was a tough six months but our neurosurgeon had to be sure. He performed another brain surgery on her January 2016 which was one of the hardest days of our lives but she is doing well. I see a therapist regularly to help me cope with our situation. She gave me the best advice. Instead of waiting for Rosie to get sick again I tell myself and anyone who asks how she is, “today she is well, if she gets sick tomorrow then we will deal with it tomorrow, but for today she is well.”
The twins just started school. I have provided info to the school about her symptoms and her care and just hope every day that when the time comes, she is looked after till we can get to her.”
Do you have any advice for parents who are struggling with TTTS?
“I think back now and know that my refusal for my delivery to be postponed saved Rosie’s life. I urge mothers in my situation, pregnant with twins that could be at risk, if you want a second opinion get one, if you want more scans, ask and get them or pay for private ones as well as the public hospital ones. And if at any time you feel strange or different, or do not agree with what a doctor tells you, trust your instincts. Like me, you could be saving your babies lives.”
Sign up for our newsletter or follow our Facebook page to stay updated on new TTTS or TAPS stories



Crystal’s Twin to Twin Transfusion Syndrome Story

This TTTS story is written by Crystal Olguin Duffy (US). Follow her on her blog The Duffy Diary.
“Oh, my gosh! There are TWO blue lines! I’m pregnant!”
I’ll never forget those words, I uttered, when I realized that I was pregnant again. My husband Ed and I had recently returned home from a surprise trip to Paris where we decided to start trying for another baby. Our 18-month-old daughter Abigail was now going to be a big sister. At seven weeks however, I began experiencing throbbing and painful cramps accompanied by strong pelvic pressure and heavy bleeding. I was sure that I was having a miscarriage. I went for an ultrasound and my doctor asked if it was a spontaneous pregnancy. I had no idea what that was. Immaculate Conception? We looked at the monitor and he told us that there were two heartbeats and two amniotic sacs—we were having twins! Ed and I were above the moon, we felt so lucky to be given this special gift of twins.”
Blood clot and bed rest
“The ultrasound unfortunately also revealed a blood clot in my uterus. It had caused the cramping, bleeding and discomfort. The doctors hoped that resting and good nutrition would do the trick and that the blood clot would reabsorb itself – and it did! I cannot describe how grateful we were. After 1 month of bed rest at home I could finally enjoy and relax the rest of the pregnancy. At around 12 weeks, we learned that we were given the gift of identical twin girls. We were so happy, but I knew that my husband and our Yorkie pup Charlie would be desperately outnumbered. I asked my husband once shortly after we found out we were having more girls, if he was okay with not getting a boy. He kissed me and asked why he needed a boy? He felt that our daughter Abby envelops anything he could have ever imagined his child to be. My heart melted and I fell in love with him all over again.”
Tragedy of TTTS
“I was overwhelmed with happiness and worked to prepare for what would soon be a very full and busy household. I was at the peak of healthy, energetic, and excitement. However, at 22 weeks I panicked. A routine ultrasound revealed that there was an abnormal amount of fluid around one of the twins. I saw how seriously the doctors took this discovery. After targeted tests were performed, I was diagnosed with Twin to Twin Transfusion Syndrome. The fear of losing our babies returned. I couldn’t wrap my mind around the tragedy of TTTS. Our babies were healthy, but suffered consequences of sharing a placenta. I was immediately referred to a specialist in high-risk pregnancies. Because our condition had already advanced to stage III TTTS, it was decided that the best treatment for us was to undergo laser ablation surgery.*”
*Laser ablation surgery aims to interrupt the blood flow in the vessels that connect the twins through the insertion of a small telescope and a laser device into the uterus. The surgeons look for the vessels that are providing the blood flow between the two babies and blazer those vessels, so blood flow can no longer happen between them.
Surgery and further complications
“Our surgery was scheduled quickly. One day after our consultation, two days after the diagnosis. The surgical team lasered 11 blood vessels and drained an excess of two liters of amniotic fluid from the recipient twin’s sac. When I returned home I had to be on bed rest to recover. That same week, we learned that despite the surgery’s success, there was a further complication. There was a hole – septostomy – in the membrane separating the twins. The hole was small in the beginning, but one of the girls tore at it, making it large enough to swim through. She joined her sister, so that they were in the same amniotic sac. I was now carrying mo-mo twins. I was placed on bed rest at the hospital because the risk of umbilical cord entanglement and compression was high. I was being monitored rigorously.”
Together again
“One of the hardest things I had to endure was being away from my daughter Abigail for so long. I arranged for visitors, friends, family to come visit me in the hospital every day. I loaded up on magazines, movies, snacks, pictures of my family and Abigail, a countdown calendar – even a lamp to make my room feel more like home. We had a barbecue, baby shower and even a surprise anniversary dinner during my stay. I went to an antepartum support group every week. I got to meet other moms in similar situations. In this group I met a musical therapist who worked with me and helped me find a creative outlet to express and deal with everything I was going through. With her help I wrote and recorded a song called “Together Again.” Not only did it help me pass the time, but it was also therapeutic in helping me process the stress, anxiety, and loneliness of going through my last month of pregnancy at the hospital.”
Dramatic delivery
“One evening at the hospital I felt sick. I alerted my nurse that something felt off. The date was 18 June 2014. By the next morning, I had full-blown contractions. I was put on magnesium to try and stop the labor. However, I dilated even more and a c-section surgery was recommended. I was so excited to meet my babies. As soon as the surgical team began they knew something was wrong. Ed, my husband, was asked to leave and I heard one of the nurses say something about a blood transfusion. I was bleeding heavily. I had had a placenta abruption.* I hadn’t anticipated that. Not once through all of my pregnancy did I think about my own life being in danger. I had remained positive and strong in my faith through it all. They managed to stabilize the situation and one of my best memories is hearing the babies scream for the first time. Their lungs were strong and healthy. A team of clinicians stood by, ready to transport the girls to the Neonatal Intensive Care Unit (NICU). Katherine Maria and Lauren Elizabeth each weighed 3 pounds (1360 grams) when they were born.”
* Placental abruption is when – in rare cases – the placenta peels away from the inner wall of the uterus. It can happen either partially or completely. It can deprive the baby of oxygen and nutrients and cause heavy bleeding in the mother. Left untreated, placental abruption puts both mother and baby in jeopardy.
The aftermath
“The girls spent 38 days in the NICU at Children’s Memorial Herman in Houston, Texas. They are now healthy, happy and rambunctious little toddlers. As I think back on all of it I still can’t believe what had to happen for us to all be here together. Despite all our complications my twin daughters and I are healthy, happy, and extremely blessed to have one another. It took not just one but a series of miracles to us to emerge healthy—we are walking miracles.”
Sign up for our newsletter or follow our Facebook page to stay updated on new Twin to Twin Transfusion Syndrome stories.



Do you have Twin to Twin Transfusion Syndrome stories to share with the readers of this site? Please write us an e-mail. We’re always looking for more parents who’d like to share their Twin to Twin Transfusion Syndrome stories.














This was very well written. Would you consider writing about those whose twin babies don’t make it? An article of grief/ healing? And those within the sub groups of TTTS? TAPS, TRAPS, TOPS, etc. I was told my twins died of TTTS. They never had the fluid difference and one came out very pale, one very red. I now think they had TAPS instead and mine (and other identical twins) should have had weekly ultrasounds AND Dopplers.
Hi Becky,
Thank you for your comment, and yes, definitely – it’s an area we haven’t covered very well (yet), and we will get there. I’m deeply sorry for your loss. If you would consider sharing your story, you’re more than welcome to reach out to me at kate@about-twins.com. Best wishes to you and your family!
Kate,
Thank you for this article, On Par with your usual work of the Highest Quality.There is a detail I believe that may be of interest to your readers, perhaps to a small group of them this could be potentially Lifesaving Knowledge: I seem to recall Crystal had Anterior Placentation, a state in which the Blastocyst which implanted then Cleaved did so on the Front (Anterior) Uterine surface. This happens perhaps 1/3 of the time in MoDi, & at similar Frequency in the Singletons. It is usually a Mere Curiosity, with no Modification to the basic risk factors of a MCDA gestation save for the fact that Maternal Movement Perception is impeded, sometimes Severely enough that Kick Counting as prescribed by UK NHS becomes Problematic, or occasionally Impossible. This normally Benign placental configuration becomes a Threat Factor if TTTS should affect the gestation severely enough that Surgical Intervention is necessary.
Then, it can Change Everything. The usual Points of Entry into the Uterine cavity are no longer valid. The Geometry of the operating field is truly distorted The Attending must be of sufficient skill to Map Out & Plot alternative ones that fit the mom,& effectively operate in a World turned quite literally “Upside Down”. Of the 41 practitioners in the US & Canada that do TTTS Laser, spread out over about 30 Centers, there are but 4 that have been positively identified as having sufficient skill in Anterior Placentation TTTS Laser such that their rates of Survival are not Significantly Hindered by the presence of this Anatomical Complication.These “Top Tier” Centers are Huntington Memorial in Pasadena CA, under Chmait, Johns Hopkins in Baltimore MD under Baschat, Denver Children’s in Colorado under Crombleholme Zaretsky & Associates, and finally Texas Fetal under Moise, Johnson & the Consortium, comprising nearly a dozen surgeons at that World Class Houston center,based at Children’s Memorial Herrmann Hospital. This is not to be confused with the group doing Fetal surgery at Texas Children’s Hospital, also in Houston.
Anterior Placentation. Usually a Triviality, taking on a Sudden & Paramount Importance should TTTS Strike.