Twin Birth Stories: Natural, C-Section & Vaginal Birth After C-Section
Read our twin birth stories and learn more about natural birth, vaginal birth after c-section, c-section for one or both twins and twin home birth. We’ll continually publish new twin birth stories. Please message us through our Facebook page or write us an e-mail if you’d like to share your twin birth story.
Twin birth stories – natural
Read twin birth stories from women who’ve given birth vaginally. Visit our twin birth page to learn more about how a natural twin birth progresses, and read about twin birth plans.
Positive twin birth stories: Mette’s twin birth story
Mother: Mette Tvilling Johansen
Children: Older brother and fraternal twin girls (born 26. February 2014 at 37+0 weeks in Denmark).

How did you feel about having to give birth?
“I was terrified when I found out that I had to give birth to twins. I have an older son and experienced his birth as awful. I was quite shaken up about how painful it was and how unprepared I felt. I did attend a birthing class at the hospital prior to his birth, but it wasn’t very good. I didn’t receive guidance on how to handle the pain mentally and physically and how to conduct myself during birth. It revolved more around different kinds of medical pain relief options. During the birth of my son, the pushing phase lasted 2-3 hours, I experienced vaginal tearing, and afterwards I kept bleeding due to placental abruption. It took a long time before I healed physically and emotionally after that experience.”
How did you handle those fearful emotions the second time around?
“I’m quite pragmatic, so I decided that I had to do something to change how I felt. I knew that I couldn’t allow myself to be as physically and emotionally exhausted the second time around. I would soon have three children to tend to. I searched the Internet and found a different birthing course. I decided to attend it even though it cost a lot of money. I knew that it was a lifetime investment.”
How did the course help you?
“The course gave me an understanding of how the body actually works for you during a birth. I was taught how to work with my body.* I didn’t understand how to do that at my son’s birth, but I did when giving birth to our girls. It would be a lie to state that it didn’t hurt, but nevertheless I’m hesitant to call the labor painful. The pain became something else, it was more like a feat of strength. I would seriously like to do it again, but my husband and I feel that we have enough children. After the birth of our girls, I understand why marathon runners or ironman participants do it more than once. If I had to rate the pain of each of my two birth experiences, they’re definitely at opposite ends of the pain scale.”
*The course is called “pain free labor” and is offered by the Danish course provider Anja Bay.
When did you go into labor?
“I had noticed light spotting around midnight, when I went to bed. I wondered whether or not it was a sign that birth was imminent. I fell asleep and woke up at 4 am in the morning doing labaro breathing exercises.* I had practiced it so much during my pregnancy, that my body could do it on its own. I still use the technique when I’m in pain, for instance at the dentist. This technique made me feel prepared -I knew how to get through the contractions. I even packed a bag between the contractions and showered. I asked my husband to call the hospital and tell them that I was in the active phase of labor. I knew that if they spoke with me, they wouldn’t believe that I was far enough along to come in. I was calm and completely in control. My friend came to take care of our son. She asked me if it’s normal to look the way I did. She thought I looked and acted too normal to be in labor.”
*Laboro is a way of breathing you can use during the active phase of labor. Among other things it’s a natural way of reducing pain and oxygenate the body optimally.
When did you arrive at the hospital?
“We walked over there. It was only a five minute walk and I felt good. I experienced 3-4 contractions on the way. We were in the delivery room at around 4.30 am and at about 6.30 am I gave birth to our girls. The pushing phase lasted less than 20 minutes. The girls were born seven minutes apart. My energy and motivation never left me and I was enormously proud of my own performance. I used the tools I received during my birthing course all the way through and my husband really supported me in using them. That helped me so much. He attended the course as well and knew how to guide me through the contractions. He told me when to get ready for a contraction, letting me know when I should use the laboro-breathing technique* and when I was halfway through. He also guided me out of the contraction.”
*When using the laboro-breathing technique you take short, superficial, rhythmic breaths.
How did you feel afterwards?
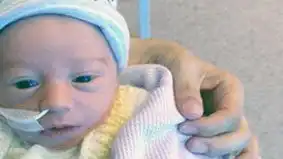
“It felt like my uterus shrink back and my stomach started to go down almost immediately after giving birth. My muscles and tissue didn’t feel knackered. I was 39 years old, and I felt like a young girl. I actually had to restrain myself, I felt so strong and energetic. We had to go to The Neonatal Intensive Care Unit (NICU) afterwards, because one of our girls was quite small. I walked over there with the babies.”
How big were the babies?
“One of our girls weighed 1800 grams (3lbs, 15oz) and measured 49 centimeters (19.29 in). The other one weighed almost 3000 grams (6lbs, 9oz) and measured 52 centimeters (20.47 in).”
Were their weights surprising to you?
“I had a very easy and straightforward pregnancy, until about two months before my due date. During most of the pregnancy, we were told that the girls weighed about the same and were following the appropriate weight scale. All of a sudden they found out that one of the girls were significantly smaller. We were monitored much more closely after this discovery. We were told that labor would be induced about three weeks before my due date instead of two weeks. Three days before I was scheduled to be induced, I went into labor by myself. This happened when I was 37+0 weeks pregnant.”
How did the following day’s at the hospital progress?
“The smaller one of our girls was being fed through a tube, but I soon began to tandem nurse. We weren’t discharged until after 3-4 weeks, but we were allowed to go home after five days in the NICU. We had frequent visits from hospital staff. It was nice to be allowed to go home. It didn’t feel right staying at the NICU. We had two healthy children, one being only a bit underweight. The other parents had children on life support and they were dealing with serious health issues.”
Would you like to share your twin birth story with the readers of this site? Please write us an e-mail. We would love to publish your story. Twin birth stories will continually be published on this site.




Twin birth stories: Stephanie’s twin birth story
Mother: Stephanie Joy
Children: One older child, identical mo-di twin girls (born in November 2008 at 37+2 weeks) and one younger child.

How did you feel during your pregnancy?
“I went to the doctor due to pain on my right side, I thought it may have been an ectopic pregnancy. The doctors did an ultrasound, and all they were able to see was a sac. I was concerned, so at 9 weeks I requested another ultrasound – that’s when I was told they saw the baby, and then they saw another baby…. TWINS! I actually felt great during my pregnancy. I lived in the city and walked all the time. I worked until I was 32 weeks. Walking started to become a bit of a struggle after 32 weeks due to pressure, but overall I felt fantastic.”
Did you experience complications?
“Yes, at 32 weeks I was experiencing contractions. I was admitted for three days. It was the worse thing I have been through. I was given magnesium to stop the contractions and steroid shots for my babies lungs. I met with doctors from the Neonatal Intensive Care Unit (NICU) to assure they would do everything they could to help if the babies were born.”
How did you feel?
“The magnesium was the worse part aside from the fear of giving birth to my daughters early on, it made me feel like I had 105 fever. I could barely see and couldn’t move. I became completely weak. I felt so defeated till the point I thought it was okay if my daughters were actually born at that moment. Nurses had to come into my room wearing coats because my window was wide open, and my room was freezing although I wasn’t. Finally day three my contractions stopped. I hadn’t had a bite to eat in days, and my body was still weak from laying down all day. My doctor wouldn’t let me leave unless I could walk out of the hospital on my own. I walked at turtle pace holding onto a wall, but I made it out. I was put on limitations meaning no more work.”
Did you do something to prepare for delivery?
“Actually I had five doctors – yes five. I told each and everyone that unless our lives were in danger, I did not want a c-section. This was the only prepping I did, I prepped my doctors. I’m glad I did.”
What were your thoughts about giving birth to twins?
“I feared many things. I think this is normal. I feared everything you usually hear, babies being born early, having to have surgery, but at the same time I felt so blessed.”
When did you go into labor?
“I was 37+1 weeks pregnant. I had a routine appointment. My doctor checked my cervix and told me “You’re 4cm, go to the hospital.” I went shopping – it sounds crazy right? But I knew these girls weren’t going to make a quick entrance, and I was three blocks away from the hospital. I went to Babies”R”Us and got them their first Christmas onesies. I don’t advise anything I did, but I know my body. I even got Chinese soup because I knew I would go a while without eating. YAY ice chips.”
How did the labor progress?
“I was stuck at 6cm from 6pm until 9am. I was given Pitocin* which didn’t work at all. I will add during the night I heard major screams in the hallway. I thought people were so happy a baby was born, but nope, Obama became president. This was such a funny moment for me. My doctor broke my water at 9am, and finally my cervix decided to do its job.”
*An induction with Pitocin means your doctor or midwife will induce your labor using a medicine called Pitocin, which is a synthetic version of oxytocin. Pitocin can be administered if you aren’t contracting quickly enough or aren’t in labor at all.
What happened next?
“I decided to get an epidural at 9cm, I know, really late, most doctors wouldn’t even do an epidural so late. I felt twin A’s head coming down as they were doing the epidural. The only reason I got it was because twin B decided to move from head down to transverse to footling breech.* I wanted to be awake just in case a c-section was needed.”
*Transverse lie means that your baby is lying sideways across your tummy. In a footling breech position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What happened then?
“I was wheeled into the operating room. I had four doctors, two nurses, the anesthesiologist and two student nurses watching at the door. I was pretty famous for a sometime. I knew when to push since the epidural was in for a short time. I pushed twin A out with three pushes, one doctor delivered her. Then my favorite doctor came to deliver twin B, three pushes, he grabbed her feet and told me when to push and when to stop pushing. My girls were two minutes apart, and they were so small. My best example of what it felt like pushing them out is a fart bubble stuck in your cheeks.”
How big were your babies at birth?
“Baby A was a peanut. She was 4lbs, 7oz (2012 grams) and 17 inches long (43 centimeters). Baby B was 5lbs, 6oz (2438 grams) and 18 1/2 inches long (47 centimeters).”
When did you leave the hospital?
“I left the hospital about three days later, but baby A was in the NICU for 12 days for jaundice and low birth weight. This part was heartbreaking, I visited her everyday.”
Any advice for future twin parents?
“Breathe. Time goes by so quickly, the fears will pass, and they grow so fast. Enjoy them, accept help, bundle your little ones up and take a walk, you’ll need fresh air. Lack of sleep doesn’t last forever, it doesn’t get easier, each stage is just a different transition, a different experience. Just love your babies, because in the blink of an eye they will no longer be babies.”
Would you like to share your twin birth story with the readers of this site? Please write us an e-mail. We would love to publish your story. Twin birth stories will continually be published on this site.







Positive twin birth stories: Sarah’s twin birth story
Mother: Sarah Naylor
Children: Older brother and fraternal twins Isabelle and Oliver (born June 2017 at 37+2 weeks in the U.K.).

When did you go into labor?
“I was induced when I was 37+2 weeks pregnant. I called in at 9 am and went in 9.45 am. They put on a monitor for an hour and then a pessary at 11.30. The monitor was removed around 12.30 and I went for a walk. I had some more tightenings so I was put back on the monitor.”
How did the labor progress?
“I needed the loo at about 5 pm. I walked to the loo where my waters started trickling. I went back onto the monitor and contractions were intense and regular so I was checked. I had dilated to 3-4 centimeter* much to the midwifes and my shock. I moved to labor and delivery at about 6 pm and had some gas and air. I managed for about an hour then asked for pethidine as I was determined to not have an epidural. Almost as soon as pethidine started to kick in the contractions were on top of each other and I shouted “I need to push” but was told no I wasn’t ready. I told my midwife to check.”
*This means that she is in active labor. Read about the phases of a twin birth.
What happened next?
“It’s a bit of a blur as my midwife pretty much went to hit a buzzer, but Oliver was already crowning and out in one push at 8.14 pm. He was born before anyone else arrived but wasn’t breathing. The room flooded, but Isabelle was already crowning and was born in one push. She was fine. Even though she was born nine minutes later and a whole lb smaller, she was the stronger twin. She weighed 4lbs, 2oz (1871 grams) and her brother weighed 5lbs, 2oz (2324 grams). She was cleaned up while I delivered both placentas really quickly. Gas and air was used as they ramped up the drip to contract down which hurt more than labor. Oliver was taken to neonatal due to his breathing issues. They were related to him being born too quickly as he was twin B but ended up becoming twin A. Unfortunately Isabelle was taken to neonatal too due to her not feeding. I’m not going to lie, I was gutted, as carrying to 37+2 weeks I had really high hopes of no separation. Three days after I’d given birth we were discharged from neonatal to transitional care.”
How do you feel about the birth?
“Overall I never imagined I could give birth to two babies with only pethidine and gas and air in three pushes overall. I only had a second degree tear to show. I can honestly say I would do it all over again tomorrow, yes it hurt, but it was incredible and I feel incredible, knowing my body knew exactly what to do and feeling everything was absolutely perfect. I wanted a mad dash to the hospital, waters breaking and spontaneous labor, but this was so much better.”
Would you like to share your twin birth story with the readers of this site? Please write us an e-mail. We would love to publish your story. Twin birth stories will continually be published on this site.

Twin birth stories: Ann’s twin birth story
Mother: Ann Mørk Røjkjær
Children: Three older boys and fraternal twin girls Ronja and Sif (born January 2014 at 38+1 weeks in Denmark).

How did you feel about being pregnant with twins?
“The twins were little surprises in many ways. They are made on birth control shortly before I was scheduled to get my tubes tied. We didn’t want more children.”
How did you react?
“Even though we didn’t want more children it took us five seconds to agree that we would keep the baby. At the first scan in week 13+1 our baby turned out to be twins. Our three older children are boys so I really hoped that our fraternal twins would be of the same sex and girls. And they were! Our boys are 7 years, 5 years and 19 months older than the twins.”
When did you go into labor?
“I was induced at 38+1 weeks. It should have been done the previous day, but we were sent home due to the hospital being overcrowded and lacking staff. When I was finally admitted, my membranes were ruptured and contractions came within a short time. A little less than four hours after my membranes were ruptured the girls were born vaginally.”
How did the labor progress?
“When twin A was born, twin B’s heart rate dropped. The medical staff couldn’t get the drip that should stimulate my contractions going. My midwife did something inside of me – I’m not sure what – maybe a sweep of membranes. Three other people were messing with my arm, trying to get the drip to work. Another was holding twin B in place, so she wouldn’t turn. Yet another was listening to my stomach with a stethoscope. It ultimately worked and I gave birth to Sif – twin B. She came out breech and born with the caul. She got a bit of oxygen and a check-up by the doctors and was then passed over to me.”
How were the babies doing?
“Sif was a bit too small. Her placenta didn’t work optimally. The medical staff hadn’t checked growth or placenta for a few weeks prior to the induction. If they had, I would have gotten a c-section due to the malfunctioning placenta, but also because she was 500 grams (1lb, 1oz) smaller than her sister. Sif weighed 2320 grams (5lb, 1oz) and Ronja weighed 2820 grams (6lb, 3oz) at birth.”
When did you go home?
“We went home the day after their birth, against the advice of the hospital. I had a short, but horrific stay at the hospital, where I gave birth. The staff was very busy and the hospital was overcrowded. I was moved to a room with four other mothers and I was lying next to an open door. It was drafty and everyone could look in while I was tandem breastfeeding. I’m so happy that we decided to go home. We only chose to do that because we were able to get transferred to the hospital in the city where we live. We got an open admission at that hospital and could drop by whenever we wanted. It’s only a five minute drive away from where we live. The only thing Sif needed to get done at the hospital was to be weighed once a day. We also needed to supplement with formula after I’d nursed her. We gave her the formula ourselves and then drove to the hospital every day to get her weighed.”
How did the first day’s progress?
“When we arrived home my milk went in immediately. My husband went and got our three other children who had been staying with their grandfather. The minute they came in the door the girls kind of “woke up.” I think they felt safe hearing the sounds they knew from inside my stomach. We were discharged after four days and three visits at the hospital. The staff was quite surprised and happy for us. The midwife, who weighed Sif, was nicknamed “My” and Sif got that name as a second first name.”
How did the following months proceed?
“Both children were admitted to hospital for about one and a half weeks when they were two months old. They had CPAP* treatment due to Respiratory Syncytial Virus Infection. Also, Sif had pneumonia and she was being observed for whooping cough. She didn’t have that, but she was almost admitted to intensive care, because she stopped breathing. I hated every second of it, but we didn’t leave the hospital a second before they asked us to. Even though the hospital was overcrowded, the staff was very competent. They didn’t have time to be in her room when she was at her worst, but the nurses moved a chair, a table and a computer in there, so they could do paperwork in her room. They could react immediately if we needed them and that made us feel very safe. Sif needed help to breath 10 times the night she was at her worst.”
*Continuous positive airway pressure (CPAP) is a treatment that uses mild air pressure to keep the airways open.
When did they sleep through the night?
“Already when they were a few days old they slept pretty well at night. They would wake up for feedings, but would fall asleep again as soon as I’d nursed them. When they were about six months old they slept from 1am to 11am, but I still had to nurse them a couple of times during that period of time.”
Any advice for future twin parents?
“If you’re unsure or nervous about something, go get it checked out. Whether it’s during pregnancy, your children being sick or you’re concerned about their development. Children are so different.”
Would you like to share your twin birth story with the readers of this site? Please write us an e-mail. We would love to publish your story. Twin birth stories will continually be published on this site.


Twin birth stories: Bina’s twin birth story
Name of mother: Bina Rosendahl Madsen
Children: Fraternal twins Darwin and Hector (born January 2013 at 34+3 weeks in Denmark)

When did you find out that you were having twins?
“When I was about six weeks pregnant. I got a scan early on, because I was in fertility treatment. We actually saw three heartbeats. They were unsure about one of them, because the baby was only half the size of the other two. My husband and I didn’t find the amount of babies frightening in itself, but we were quite nervous about the risks a triplet pregnancy pose. There was no doubt in terms of what the doctors recommended. They told us to get a fetal reduction, because a triplet pregnancy would be way too dangerous. However, we were told to let a few weeks pass, because the smaller baby might vanish on its own.”
What happened at the subsequent scan?
“There were only two heart beats left, when we went back in week 9. I didn’t feel the miscarriage physically, but we felt very ambivalent emotionally. We had decided that we would keep all three of them. We were sad, but we also knew that the risks associated with this pregnancy now was significantly lower.”
How did you feel in your first trimester?
“I felt very nauseous and exhausted. I had something to eat right before I went to bed every night, but woke up hungry at 4 am. I got out of bed and had a rye bread porridge. After my first trimester I started feeling better and could still go running. Then pelvic girdle pain kicked in. In combination with a lot of braxton hicks contractions it resulted in me needing to go on sick leave in week 20.”
Did you experience any other complications?
“Yes, this was only the beginning. In week 23, I had an internal scan where the length of my cervix was measured. The scan is standard for women carrying twins. My cervix was on the verge of being too short and the doctor told me to go home and rest. When I went home I was uncertain about what resting entailed, so I wrote another doctor. She called back and wanted to see me for another scan four days later. At that scan, my cervix had shortened even more. The doctor decided to admit me to hospital and put me on bed rest. By then I was 24+0 weeks pregnant.”
How did you feel about that?
“I was surprised. I didn’t expect to have a complicated pregnancy. I exercise a lot and feel good about my body. I have faith in my body and felt that it could handle the pregnancy.
I was only in the hospital for about two weeks, when I was transferred to a larger hospital. This happened because one of the fetal membranes was close to passing through my cervical pessary. The cervical pessary was inserted to support my cervix and reduce direct pressure from the uterus on the cervical canal. If the fetal membrane passed through, my water would break and I would go into extremely preterm labor. There was nothing the hospital staff could do at this point, but monitor me, and keep giving me medication to counteract the braxton hicks contractions.”
Did you go into labor?
“No, I continued being on bed rest. It’s an awful feeling not knowing if you’ll give birth within the next two months or the next two hours. I had trouble concentrating in general, because I felt I was on the verge of giving birth all the time. I was overly conscious about every signal my body was sending. It was a constant battle having to stay in bed. When I stood up to go to the bathroom, I felt like I was risking the life of my babies. I knew that it could be the extreme consequence of me getting up. I wasn’t in the best mood, I was frustrated.”
Was there anything that made bed rest more tolerable?
“We didn’t have other children, so my husband could be there with me a lot. He worked only a few minutes away from the hospital, so he usually visited me in the morning and in the evening, when he got off work. If we had an acute scan, he could usually be present. I had a lot of visitors, family and friends, which helped.”
How closely were you monitored?
“They checked my babies heartbeats every day. I took blood thinners and needed help with the injections. The babies were scanned twice a week and their heart rhythms and flow were monitored. They were growing as they should. At one point I had a conversation with a pediatrician who informed me about extremely preterm babies. He told me that if they were born in week 24, they would have a 50 percent chance of making it. He also talked about the risk of infant brain damage and other complications. He said it could be a good idea to have names ready in case our children would need an emergency baptism.”
How did that knowledge affect you?
“I was glad to have the conversation, because I didn’t know what a preterm labor entails. I knew that the babies would be very small, but I was not aware of what it meant in terms of survival chances and short and long-term health effects. I realized that during our conversation. It kind of knocked me out. Prior to our conversation, I had been singing songs and cuddling my stomach. I stopped communicating like that for a while. I tried to distance myself, to prepare myself for a possible loss. I wasn’t nervous about how the babies were doing in my womb, I could feel them kick every day. I was scared about giving birth to them too soon and losing them.”
What helped during those weeks?
“My husband and I were good at talking about it. I always had the feeling that we were in this together. We had set a few milestones to celebrate. When I reached week 28 he brought cream puffs to celebrate. It helped a lot that he came by every day.”
Looking back, how do you remember your pregnancy?
“Like hell. I feel very cheated. I didn’t have many weeks where things were quiet and calm. I missed the joy of nesting, buying children’s clothes and decorating the nursery. It would have been great with a little more time to myself. I would have liked more time to prepare myself for the new role of being a mother in a quiet and calm way.”
Did you stay on bed rest until labor?
“No. Around Christmas I was allowed to go home for a few days. My condition was stable in the sense that my cervix hadn’t shortened further and the braxton hicks contractions were manageable. The doctor knew there was a risk of preterm labor, but also focused on the risks of me continuing on bed rest. I was getting bed sores on my feet and the risk of blood clots were also present. I was home for about two weeks, but woke up one morning looking like the Michelin man. My body was swelling and I had a headache. I went to the hospital and they discovered that my blood pressure was high. They also found protein in my urine. It was preeclampsia. I was admitted to hospital again.”
How did you feel?
“I felt awful. I didn’t expect that I would be admitted to hospital due to my blood pressure. It had been fine all along. Now my blood pressure was suddenly fluctuating. It was extremely high and then a little too low. When it was fluctuating, I felt like I was having the flu.
I was discharged again on a Sunday afternoon, and went home for a day. Then my water broke at 7 pm Monday. I was okay with that. I was feeling really sick due to preeclampsia. My whole body was hurting. My mother and grandmother both had good experiences giving birth and I was looking forward to experiencing it birth myself.”
How did the labor progress?
“We live close to the hospital and were admitted at 7.45 pm. I was in active labor* around 11 pm. The pain was overwhelming, it was tougher than I’d imagined. I didn’t get an epidural – I had made it clear that I didn’t want one. I used nitrous oxide as pain relief during labor. I remember asking for a c-section at one point. That was not an option. The birth was progressing as it should and the babies were doing fine. There were only me, my husband, the midwife and an assistant present. It was more quiet and calm, than I thought it would be, which was a nice experience.”
*You’re in active labor, when your uterus is dilated 3-4 cm. Read more about the phases of birth.
What about the pushing phase of labor?
“A lot of people were summoned. I can’t remember how many, but there must have been at least 10. Darwin and Hector were both positioned perfectly. Nevertheless, I was fighting quite hard giving birth to Darwin, because I never physically felt the urge to push. Regardless, I pushed and pushed and pushed and when I succeeded in giving birth to Darwin, he went over to my husband. A doctor almost attacked my stomach, holding it tight, so Hector wouldn’t turn. He wanted him to stay in the perfect position he was in. Darwin was weighed, washed and placed on my chest. When I felt a contraction and they told me to push, I remember telling them to move Darwin. I couldn’t grasp giving birth to Hector, while Darwin was lying on me. Hector was placed directly on my stomach. He was born 3 minutes later at 3.26 am.”
How were the babies doing?
“They were doing fine. They both screamed, when they entered the world. Hector was a bit affected by a small decrease in his oxygen level at the final stage of birth, but nothing major. Darwin weighed 1990 grams (4lb, 6oz) and measured 46 centimetres (18.11 in). Hector weighed 1,813 grams (3lb, 15oz) and measured 44,5 centimetres (17.52 in).”
How did the following weeks progress?
“The children had a few minor difficulties due to being born preterm. They couldn’t eat by themselves, had trouble keeping warm and had infant jaundice. They were in the Neonatal Intensive Care Unit (NICU) for 3,5 weeks. Darwin was emitted briefly again because of dehydration. He had a few issues nursing, but they were quickly resolved. While Darwin basically was content and slept most of the time, Hector suffered from very severe acid reflux. He cried a lot. It was extremely hard. He couldn’t lie down and sleep, so my husband was sitting up in bed with Hector, who slept on his chest for the first 4 months. The hospital gave him a lot of medicine, but his stomach couldn’t cope and it didn’t help.”
Did you try an alternative to medicine?
“We took him to an osteopath.* He found a lot of tension in Hector’s neck, pelvis and back. He told us that these areas were connected to the ring of muscle – the lower esophageal sphincter – that in Hector’s case was allowing his stomach contents to leak backward from the stomach. The osteopath worked on him, but it didn’t have an affect. After two months he told us that he was close to throwing in the towel, but that he would give it one last try. He suggested an intensive treatment, where we would have to come in every day. On day four he said that he thought he had solved the problem. We took Hector home and from that day on he slept through the night in his own bed. We were so happy, but also frustrated. He had been screaming bloody murder for the past four months and we wondered why somebody didn’t offer him relief sooner.”
*An osteopath emphasizes massage and other physical manipulation of muscle tissue and bone.
When did they sleep through the night?
“When they were about 9 months old. I could put them to bed at 7 pm and they would sleep until around 6 am. It started getting easier, when they were about 6 months old. They developed a steady rhythm.”
Any advice for future twin parents?
“Lower your level of ambition in regards to what you can do with two children in the beginning. Especially when they’re born preterm. I really wanted to take them out in their pram and do things like attend baby hymn singing classes and a group for new mothers. I also wanted to tidy up the kitchen and clean the feeding bottles before my husband came home. If I was doing it over again, I would spend the first three months at home in bed, watching television and focusing on breastfeeding and getting as much sleep as possible. The other stuff doesn’t really matter in the beginning.”
Would you like to share your twin birth story with the readers of this site? Please write us an e-mail. We would love to publish your story. Twin birth stories will continually be published on this site.





Twin vaginal birth after c-section
It’s definitely possible to give birth to twins vaginally even though you’ve had a c-section previously. However, the vast majority of doctors will only allow a vaginal twin birth if twin A is head down. Twin A refers to the twin located lower in the womb. That’s the twin who’s most likely to be born first. Look at this Israeli study as well as this U.S. study about women attempting a vaginal birth after c-section (vbac).
Twin birth stories: Lisa’s twin birth story
Mother: Lisa Krnyaich
Children: Older brother Levi and identical mo-di twins Jason & Craig (born in January 2014 at 31+6 weeks in the U.S.).

When did you find out that you were having twins? How did you react?
“My husband and I found out when I was at my first OB appointment at 8 weeks that we were having twins. My husband saw two white dots on the ultrasound screen before the doctor, since the screen was facing towards us. The doctor moved the screen toward her, and she confirmed it. We were in TOTAL SHOCK! She went on with the ultrasound, and my husband said he had to sit out in the waiting room. While he was out there he told everyone in the room. When I came out, everyone was telling me congratulations.”
How did you feel during your pregnancy? Did you experience complications?
“I was 39 when I was pregnant with my twins. I felt fine, except I had some bad heartburn. I did get winded some when I’d walk around in stores. I didn’t pass my 1 hour glucose test. I failed by 1 point. I took the 3 hour test and failed again. I guess I had gestational diabetes. I was referred to a diabetic counselor. I was prescribed a glucose meter and strips and told to check a few times a day. I kept track of my readings for a week or so and was prepared to discuss them with the counselor, but my water broke unexpectedly on January 3, 2014. I was 31+2 weeks pregnant.”
When did you go into labor?
“I woke up early on January 3rd to go to the bathroom. My hips were hurting so badly at that point in the pregnancy that I was sitting on the edge of the bed to help with the pain before I laid back. While I was still sitting on the bed, I had what I thought was another urge to go to the bathroom. I stood up and took a couple of steps toward the bathroom and my water broke. My husband was sleeping in the bed. I woke him up and told him my water broke. I believe he asked, “Are you sure?” I wasn’t due until March 5th, so we didn’t have a bag packed for the hospital.”
How did the labor progress?
“At about 4:00am he drove me to the hospital where my OB/GYN was. I was hooked up to fetal monitors and was told by several nurses and perhaps a doctor that I’d be having the babies that day. I had read several things on the internet that women had had their water break and they had their baby/babies days or even weeks later, so I wasn’t sure why I was told that I would have the babies that day. One woman examined me, and I was several centimetres dilated. That’s when the decision was made to transfer me from the hospital I was at (Wheeling Hospital in Wheeling, West Virginia) to a bigger hospital that had a Neonatal Intensive Care Unit (NICU), since Wheeling didn’t. I was transported via ambulance to West Penn Hospital in Pittsburgh, Pennsylvania. I was given a steroid shot at Wheeling before being transported, to help the babies’ lungs develop. At West Penn, my labor was stopped once.”
When did you go into labor again?
“I started to go into labor again the evening of January 6th. Pretty early on, I was offered an epidural and gladly accepted! I was able to relax and tried to get some sleep, but I had nurses and doctors coming in every few hours. The next morning I was checked and told I was fully dilated. I was offered the opportunity for another c-section or a vaginal birth after c-section (VBAC). I opted for the VBAC. I was wheeled into the delivery room where there were 21 nurses, doctors and students! We weren’t told how many people would be in there and were shocked! I couldn’t feel anything below my waist, and, therefore, couldn’t tell when I was having a contraction. I was told when I was having a contraction. I was told when I was having one and when to push. Baby A (Jason) was born at 10:48am, and Baby B (Craig) was born at 11:03am on January 7, 2014. Jason weighed 4lbs, 9oz (2069 grams) and was 17 1/2 inches long (44,5 centimetres). Craig weighed 4lbs, 10oz (2097 grams) and was 16 1/2 inches long (42 centimetres).”
How were your babies doing?
“They both needed some oxygen for a day or two and needed to be in an incubator for about a week or so. They were NICU feeders/growers. They were in the NICU for 28 days. I think I went home on January 9th. They came home on February 3rd.”
Would you like to share your twin birth story with the readers of this site? Please write us an e-mail. We would love to publish your story. Twin birth stories will continually be published on this site.




Twin home birth stories: Jessica’s twin birth story
Mother: Jessica Evershed
Children: Older son and identical di-di twin boys (born at 37+5 weeks in 2008 in the U.K.).

What were your feelings about giving birth?
“On getting pregnant for the second time in November 2007, I reflected on my experience of the birth of my son in June 2006. I had an induction for post-dates/large baby from scan/leaking waters followed by an emergency caesarean after no progress with an Occiput Posterior (OP) baby.* I had not thought a lot about it until I got pregnant again, but when I considered it, I realized it had actually been a deeply unpleasant experience that I wished to avoid repeating.”
*When a baby is head-down, but facing your abdomen, the baby is said to be in the Occiput Posterior.
What did you do about it?
“A friend had had two home births and recommended her independent midwife. The prospect of avoiding a repeat of the various traumas associated with hospital birth seemed very attractive. At £3,500 for antenatal/postnatal care and the birth itself, it was a big undertaking: it was the sort of money we could have spent on a very nice family holiday, and we decided to see it as an alternative to that – as it turns out it really was the best holiday we never had…. After meeting her just before Christmas 2007, we decided to engage her services and arranged my booking appointment with her for January, after I would have had my first scan.”
How did that scan go?
“We went for the 12 week scan on January, 5, 2008, and had the shock of our lives to discover that I was carrying two babies. This threw my plans about a home vaginal birth after caesarean (VBAC) birth into disarray, and the possible complications and dangers of a twin pregnancy seemed overwhelming. We had to decide whether it was worth taking up the antenatal care that my midwife offered, as the likelihood seemed that I would have a hospital birth at which she could only be an adviser to us at best; and possibly premature birth and/or repeat caesarean. After much thought I decided that I still wanted to have her, as the benefits of continuity of care in my situation seemed even greater, so this swung it for us.”
How was your pregnancy?
“The pregnancy went very well. It was of course hard work and towards the end I didn’t feel up to much at all but most importantly everything seemed healthy and there were no complications. I was lucky that my twins were Dichorionic-Diamniotic ruling out some of the more dangerous complications of twin pregnancy.”
What were your thoughts about giving birth?
“At 35 weeks my midwife and I discussed home birth. She was not encouraging me to have a home birth and made it clear there were additional risks with the birth of twins, wherever they were born. She made it clear that I had to understand those risks to entertain the idea of birth at home in this situation. She indicated that if everything continued so well it would be a possibility that she was willing to entertain, if that was what I really wanted – as long as I went into spontaneous labor, I was past 37 weeks, and the labor proceeded normally. The main advantage for me being, of course, that I would have my trusted midwife in control of things at the birth: allowing me more of a chance to give birth normally.”
How did you prepare?
“I had written an extensive birth plan to cover all eventualities at hospital, and I had done a lot of research into all the risks and details of what I was hoping for at my birth, both for twin birth and VBAC; so I was going into this with my eyes open. I knew the likelihood was that in the hospital I would end up with interventions I did not want, leading easily to a rushed, out-of-control situation resulting in a caesarean after all, even with the best care and strongest conviction on my part that I could refuse any intervention I did not want.
My hope was not to be governed by time limits on the gap between twins, protocols on monitoring and epidurals, and a huge audience of medics at my birth – my books gave a long list of those who ‘would’ be present at a twin birth.”
Why were your thoughts on a home birth with twins?
“Another reason for me wanting to avoid over-medicalisation was my experience aged 21 of four days in ICU with Meningococcal Septicaemia. Being bed bound and attached to tubes and monitors was a situation not to be repeated in a hurry. Because of all this I made the decision not to rule out the possibility of home birth, and it was agreed that if my midwife’s backups were available at the time, a home birth could be an option. I did think I would want to be in the hospital though, but was glad to keep my options open – and indeed remain at home during labor perhaps longer than otherwise.”
When did you give birth?
“Because of the normal procedure* with twins being to schedule a c-section or induce if babies do not appear by 38 weeks, I was keen to get things going before I had pressure to make decisions about intervention (although my consultant was happy to see me at 39 weeks instead as my scans indicated all was well), so I booked reflexology and acupuncture for the week after I was 37 weeks. I saw my midwife on the Wednesday morning at 37+5 weeks and was 3 cm dilated. Though she was cautious, she did say I was ‘ready to go’ with both babies in “launch position.” She also said that twin B was now head down, which was good news as he had been breech for a while (though both my midwife and my consultant at hospital were happy for vaginal birth to go ahead if the second baby was breech).”
* The procedure differs depending on the country you give birth in and the doctor you’re seeing. Many doctors recommend that you get a caesarean section or induction at least 2-4 weeks prior to you being full term with twins. Read more about what full term for twins mean.
What happened next?
“I had a relaxed day, and did feel some irregular tightening, but nothing major. I had an appointment for acupuncture at 4.30pm, and when I came out at 6pm I was having irregular mild contractions. My mom was staying to look after my 2 year old, and she and my partner started cooking. I was in the living room thinking ‘I don’t think I’ll make dinner’. By 7pm contractions were strong and very frequent, and my partner called the midwife soon afterwards. I started to use my TENS machine, and almost immediately had to move to level 11 (max) on the scale.”
When did the midwife arrive?
“She arrived at 8.45pm. I was having almost continuous contractions (and in the back of my mind I was thinking, ‘Oh dear, this is quite hard work, I hope it’s not going to go on like this all night’ – my only moment of doubt), and my waters had broken. On inspection, she said I was 9cm dilated, and I had to either stay home or go into hospital immediately! Getting into a vehicle and making it to hospital just did not compute at that point, and I managed to murmur ‘stay’ – I just could not imagine going anywhere. I think my mum and partner were pretty shocked by this turn of events. My midwife took this in her stride and set up all her equipment for the birth and called her backups.”
How did the labor progress?
“Luckily the other two midwives were available, and arrived within about 20 minutes, and I was pushing by about 10ish. We tried lots of positions as twin A was OP, and it was difficult to get him moving down. Eventually, we found the right position and he began to move down easily and arrived shortly thereafter. He was fine, and after waiting for the cord to stop pulsating it was cut, and dad had him skin to skin with a heating pad. I was exhausted, it was like I’d run a marathon, and was then having to start again…. but I was so elated that one baby was here that I was set to get on and go again.”
How did the birth of twin B go?
“I started contracting again after ten minutes or so, and then pushing after 30, after some confusion because his membranes had not broken and no presenting part could be seen, it turned out baby 2 had turned to a breech position. We tried a lot of positions to get him moving down and finally found one that worked. Then he came easily, almost textbook birth right up to his chest. His arms were raised above his head so the midwife had to gently manoeuvre them down and out and then he came. He yelled immediately and was absolutely fine, and I took him immediately. We left the cord pulsating for a minute before I was able to cut it. My midwife later explained that he had been flexing his legs and wriggling around before his arms and head were born, an instinctive attempt to twist his arms free aided by gravity. She only helped when it became obvious he wasn’t going to manage on his own.”
How long did the labor go on?
“I couldn’t believe that it was only 1.45am, yet there we were happily at home with the successful birth of our two boys. My labor had started at 7pm – and it was all over less than 7 hours later. I was keen for a natural birth of the placentas if all had gone well, so we waited for a bit to see if they would come out, but I had the syntometrine injection after about 20 minutes. The placentas came with some help from the second midwife who had taken over for the third stage. The placentas were fused into one and quite enormous. I had a normal blood loss and there was no worry with the third stage. The placentas were kept for us to look at later on – which was fascinating.”
How were you feeling?
“After a bit of recovery time, the midwives helped me into the bathroom where they had prepared a bath and lit candles. So, at 4am we had a little party in our tiny bathroom with midwives, Dad and Grandma – and the babies floated in the bath with me – our two year old was fast asleep. After this lovely time to allow my babies to revisit the environment prior to birth, with me floating in warm water, we returned to bed. On advice from the midwife, I lay back comfortably in bed and one by one got each baby to attach and successfully breastfed simultaneously. This went much easier than I ever could have expected. After cups of tea and chocolate biscuits the midwives packed up and left me and my partner to stare at our babies all night!”
How do you feel about the birth experience at this point in time?
“This was a truly an amazing experience, and I feel very lucky indeed. The babies are amazing, and identical, and are now about to leave primary school. I am aware that I am unusual in choosing this path, and a lot of women would consider it a brave (or even risky) option, but for me it was absolutely the right choice. I think that I was privileged to benefit from the immense knowledge and experience of my midwife, and I am almost certain that in my situation a hospital birth with monitoring and epidural would have resulted in a repeat c-section and a much more traumatic (and risky) experience all round: a back-to-back and a breech baby would not have birthed normally without movement on my part and expert help from a confident midwife with knowledge of my pregnancy and experience of breech births. I feel that continuity of care and the guarantee of experienced professionals made my birth a safe option for me.”
Would you like to share your twin birth story with the readers of this site? Please write us an e-mail. We would love to publish your story. Twin birth stories will continually be published on this site.




Twin birth stories – c-section
There is a greater risk that you’ll have a c-section if you’re pregnant with twins compared to a singleton pregnancy. It depends very much on how your twins are positioned in your womb. Some doctors will only allow a vaginal twin birth if both twins are head down. Others are perfectly fine with a twin vaginal birth as long as twin A is head down. Twin A is the twin closest to the birth canal, and the one who is most likely to be born first. It also depends on your health, the course of your pregnancy and how your twins are doing. Read more about having a c-section with twins.
Twin birth stories: Liselotte’s twin birth story
Mother: Liselotte Wiberg Larsen
Children: Identical twins William and Victor (born January 2013 at 32+0 weeks in Denmark).

When did you find out that you were having twins?
“I had my first scan, when I was in week 6. I needed to know for sure that there was life inside of me. I’d been pregnant once before, but lost my son in week 38 due to early SIDS. My children’s father and I were a bit surprised that we were having twins, but not very. There are a lot of twins in my family and we had joked about us having twins as well. Nevertheless, it surprised us to learn, at a scan in week 12, that we were having identical twins. We were sure that they would be fraternal, like by big sister’s twins.”
What else did they tell you at that scan?
“We were told that the babies shared a placenta and the outer fetal membrane. They had their own separate inner membrane.* We were told that I would need a scan every two weeks in order to make sure that they didn’t develop Twin to Twin Transfusion Syndrome. We hadn’t heard about the disease. It was very reassuring to be monitored closely.”
*This makes them mo-di twins. Read more about how identical twins are formed.
How did you feel in your first trimester?
“I was very nauseous and vomited quite a lot. I went on sick leave in week 8 or 9. I was very tired and couldn’t really focus. I got some pills from my doctor, but they didn’t help. I had biscuits next to my bed and brought food with me wherever I went. I had to relax a lot, whenever I did something, I became dizzy. I could do a bit, for instance participate in a family member’s birthday, but I couldn’t go shopping or anything else that tired me physically. I wasn’t surprised about that. I experienced the exact same thing in my previous pregnancy.”
Did you feel better at some point during your pregnancy?
“Yes. Around week 15 I started feeling better. I wasn’t so nauseous and I didn’t tire that easily. The dizzy spells improved. However, I took good care of myself and was very careful not to do too much.”
Did you experience any complications during your pregnancy?
“Yes, but not until week 27. In week 27 the hospital staff found out that William’s umbilical cord didn’t connect well to the placenta. This resulted in him not getting enough nourishment. His body tried to counteract by draining a vessel in his brain of nourishment. This could result in brain damage. They monitored me weekly, when they discovered it. Victor, our other son, wasn’t affected by it and was doing well.”
How did the following weeks progress?
“In week 29 I got medicine to speed up our babies lung development. The doctors knew that they would be delivered prematurely. I was scanned twice a week at this point. The children’s father and I were eager to have the babies delivered. We were scared, because they couldn’t do anything to help William, as long as he was still in my womb. I told the doctors to take them out, no more children should die inside of me. In week 31 we were told that they would do the c-section, when I was 32+0 weeks pregnant. This was the week where our children would no longer be considered very preterm.”
Did you do anything to prepare for the delivery?
“We visited the Neonatal Intensive Care Unit (NICU) a few days before the delivery. We saw the incubators and they explained to us, that this was where our sons were going to stay. We were also told that I shouldn’t expect to see them in the delivery room. That was quite hard to learn, but of course I understood. They needed to focus on helping our children. It was a good visit and we received a lot of useful information.”
How did you feel on the day of the c-section?
“I wasn’t nervous. I felt that we were in good hands. We went to the hospital at 7.30 am, but had to wait until 2.30 pm. That was a bit tough. I was fasting and very hungry.”
How did the c-section progress?
“Our children were delivered 3 minutes apart. William didn’t have any amniotic fluid left. The doctors struggled a bit getting Victor out, but nothing major. The children’s father and I knew roughly how big our children were, due to the many scans, I had in the last few weeks prior to the delivery. Nevertheless, the doctors, who received the babies, didn’t. They were quite surprised, the children were much bigger than they anticipated. William weighed 1580 grams (3lb, 7oz) and measured 39 centimetres (15.35 in). Victor weighed 2065 grams (4lb, 8oz) and measured 46 centimetres (18.11 in). The doctors thought that the children would each weigh around 800 grams (1lb, 12oz). For some reason they had received old weight indications from a scan done many weeks prior to the delivery.”
How were the babies doing?
“We got to see Victor briefly, William needed a bit of oxygen. They went to the NICU almost immediately and their father went with them. We had been told prior to me giving birth, that even though William was the one struggling in my womb, he would probably be the one who would do best after delivery. Victor had been living the sweet life in my stomach and would need time to adjust.”
How did the following weeks progress?
“We were in the NICU for 6 weeks. In the evening on the day of his birth, Victor went on life support. It was tough to watch him. He seemed completely gone, he didn’t make sounds or cry like William. He had a tube in his mouth and a drip in his hand and in his navel. When he was removed from life support, he got CPAP* treatment like William. William lost 200 grams (7oz) and weighed 1300 grams (2lb, 13oz). I thought that he was very small, almost unmanageable. I felt like he could break. I was allowed to hold them after a couple of days.”
*Continuous positive airway pressure (CPAP) is a treatment that uses mild air pressure to keep the airways open.
What worried you the most during the weeks in NICU?
“The alarms that kept going off and also the other children around us. While we were admitted, there were another couple who had twins much smaller than ours. They weighed around 700 grams (1lb, 8oz) and died two days apart. It affected us, even though our boys were responding positively to treatment. What if they took a turn for the worse? However, doctors and nurses assured us that they were doing fine.”
How did feeding them go?
“It was difficult teaching them to eat probably. We used baby bottles with expressed milk. Victor eventually had formula and William continued getting my expressed milk, because he was smaller. It was tough to prepare around 16 bottles a day while having to express milk several times a day. I did it for the first three months and then shifted to formula.”
What about the first weeks at home?
“Our children pretty much slept and eat for the first few weeks. They slept 3-4 hours at a time. The first few nights I went over to their crip a lot, checking if they were still breathing and doing okay. When Victor was about 3-4 months old, he had a heart scan, because a previous scan had shown that his ductus arteriosus wasn’t closed.* It had closed, but they saw something strange around the aorta. We were afraid that there was an issue with his heart. Luckily it turned out to be false alarm, nothing was wrong.”
* In infants born at term, the ductus arteriosus normally constricts after birth and becomes functionally closed by 72 hours of age. In preterm infants, however, closure is delayed.
Looking back, when did you struggle most having twins?
“When they were around 6 months old. They slept 15-20 minutes at a time, both during the day and at night. They took turns waking up. It was extremely hard. I was told that it’s due to them being preterm. They’re almost four years old now and it’s better, but they still wake up a couple of times every night. They need to know that I’m there and then they fall asleep again.”
Did you do anything that helped you through that tough time?
“Where we live, families with young twins are offered free help from the local government.* Earlier on I had turned them politely down, because I thought things were going well. But I contacted them again when the children were six months old, and asked if it was still possible. They sent a lady who came 3×3 hours a week and entertained the children. That was a big help. I could go to the doctor or dentist without them and prepare dinner in peace. She helped us for 3-4 months.”
* Some – not all – local governments in Denmark offer free help to families with young twins.
Looking back, if you could do anything different, what would that be?
“I would hire a house cleaner and ask for more help from my family. Looking back, I wish that I’d asked them to take the children for a few nights during the weekend, so my children’s father and I could have nurtured our relationship. I felt bad asking family members for help, because the children had so much trouble sleeping. I felt that it was my choice to have children, so why burden others. I didn’t feel comfortable asking them, but that’s on me. I think they definitely would have said yes, if I had. My children’s father and I split up in January 2016, when the children were 3 years old. Of course there were other issues as well, but not taking good enough care of the relationship contributed to it.”
Any advice for future twin parents?
“Nurture your relationship, remember to be a couple. Get a sitter for the children, if you feel exhausted. I’ve learned that there’s no shame in that. You need to continue living your life and not be tied down 100 percent. That’ll run you down, especially if you’re not getting any sleep. Let the mess be and don’t fuss over cleaning.”
Would you like to share your twin birth story with the readers of this site? Please write us an e-mail. We would love to publish your story. Twin birth stories will continually be published on this site.






Twin birth stories: Trine’s twin birth story
Mother: Trine Lambæk Bøgh
Children: Fraternal twins Ingeborg and Alfred (born via c-section 7 January 2011 in Denmark – due date 22 January).

When did you go into labor?
“My planned c-section was scheduled to take place 10 January. At an exam about a month before my due date, I was told that our daughter was in a transverse lie. However, at an exam a couple of days prior to the scheduled c-section, they found out that I had elevated liver enzyme levels. I was admitted and scheduled to have a c-section the following day.”
How did you feel about not being able to give birth vaginally?
“I’ve always wanted to experience the pain associated with childbirth, but generally I take things as they come, so I quickly came to terms with it.”
How did you experience the c-section?
“I wasn’t scared or anxious prior to the c-section, but I became scared when entering the operating room. I’d never seen an operating room before, it was very sterile and it reminded me of a slaughter house. I felt very overwhelmed due to all the people present. I didn’t expect 9 people. The presence of them all made me anxious. I thought about why there had to be so many, was it because it was dangerous? However, I quickly noticed that they all had a function. That calmed me. It was a little bit like an anthill – every ant had a task and they were very skilled at what they were doing.
I also didn’t know that my arms would be strapped out to the side. I remember feeling like I was being crucified.”
How did the c-section progress?
“When they were done with the preparations and I’ve had an anesthetic, they put a cloth up over my chest so I couldn’t see the operation. My husband was sitting with me. I heard the doctor say that they would start the procedure. It wasn’t painful, but I felt like I was a human bouncing ball. It was a very strange feeling. It felt like grown people were jumping up and down on my stomach, but I felt no pain. Then I heard our daughter scream and she wasn’t even out of my stomach yet. That was surreal. They had opened me up and she was screaming in there. Her brother was born two minutes after her delivery.”
Did you see them right away?
“No, they were both carried away, so I didn’t see them. It was very strange not seeing them. I knew beforehand that they wouldn’t be handed over to me right away, but we hadn’t talked about where they’d go and who would go with them. I had faith in the fact that the hospital staff would guide me through, and that the children would be given to me when they were ready. It was a huge relief getting them out, hearing them cry and learning that they were healthy and well-formed. After a few minutes my husband came back in with both of them, but they were wrapped, so I could only see two blankets. I was able to hold them later in the recovery room.”
How big were the babies?
“My daughter was 2600 grams (5 lb, 11 oz) and measured 47 centimetres (18.50 in). My son was 2,800 grams (6 lb, 2 oz) and measured 49 centimetres (19.29 in).”
How did the following day’s progress?
“We were at the hospital for about 4 days. Our daughter lost too much weight, so I needed a bit of help to make sure that the breastfeeding was properly in progress. Also, I had a very low blood count. During the delivery I lost about 1,5 liters of blood. I was on the verge of needing a blood transfusion, but I managed without. I was surprised about how much pain I felt after the c-section, but otherwise the first few weeks went on calmly. I remember thinking that it wasn’t hard to have twins at all.”
Did you keep thinking that?
“I felt it was pretty easy having twins, until they were about 3 weeks old. Then our daughter got colic. She would begin crying at around 6.30 pm and would cry on and off until 4 am. This affected our boy, who I think was upset about her crying and our lack of presence, so he cried a lot too. It was a tough time. It lasted until the children were about three months old and basically stopped from one day to the next. Then it started being much easier again. However, I never got to the stage where I felt it was relaxing to be on maternity leave. It was straining never being able to be fully present with one child, because the other one was always craving attention.”
When did they sleep through the night?
“When they were 6-7 months old. I could put them to sleep at about 7.30 pm – nurse them at 11 pm, when I went to bed – and they’d sleep until morning.”
Any advice for future twin parents?
“It helped me a lot to get them on a sleep and feeding schedule. However, twins do have different circadian rhythms and different needs in regards to feeding and sleep. Sometimes I think about whether I was being too rigorous, but on the other hand if I didn’t put them on a schedule, I’d risk one of them waking up when I was feeding the other, and then I wouldn’t be able to tend to that twins needs right away. I breastfed for a full five month and partly until they were 12 months old, so it was important for me to get them on a schedule in order to have just a little bit of free time.
Also, say yes to all the help you can get. If people offer to drop by with dinner or a cake, when they visit, let them.”
Looking back, if you could do anything different what would that be?
“We were very determined not letting the babies sleep in our bed. We didn’t want them to develop bad habits, not being able to sleep by themselves. I think we could have relaxed a bit and made things easier for ourselves, if we’d allowed them to sleep in our bed from time to time.”
Would you like to share your twin birth story with the readers of this site? Please write us an e-mail. We would love to publish your story. Twin birth stories will continually be published on this site.



Twin birth stories: Louise’s twin birth story
Mother: Louise Sandie Schmidt Holm
Children: Older brother Viktor (born 2009) and fraternal twins Felix and Liv (born April 2013 at 33+2 weeks in Denmark)

When did you find out that you were having twins?
“I knew for sure, when I was about 6 weeks pregnant. I got an early scan, because I was in fertility treatment. However, I had a hunch prior to the scan. There were a few signs, that indicated, that I might be carrying twins. I had an early positive pregnancy test and I felt very nauseous.*”
*Some women pregnant with twins have elevated hCG-levels and can test positive very early in their pregnancies. Substantial hormonal changes can also cause more severe pregnancy symptoms, like nausea. Read more about twin pregnancy symptoms.
How did you feel in your first trimester?
“For several weeks I was quite affected by round ligament pain. I’d never experienced that kind of pain before, even though I have an older son. I thought that something was wrong. The pain felt like contractions in my stomach. I was told that it’s normal when you carry twins – the ligaments need to stretch more in order to make room for the children. I had no appetite and was feeling really nauseous.”
What about your second trimester?
“I felt much better physically. The round ligament pain and the nausea subsided.”
Did you experience any complications?
“Yes. When I was in week 17, I woke up one night around midnight. I felt something gushing out of me. It felt a little like I was peeing. I sat up and took my panties off. I called out for the children’s father, who was still up, and told him that I thought something was wrong. He told me that I was probably just peeing and helped me change the sheets. He went to bed as well, but after about 15 minutes I felt it happening again. I started crying and we called a doctor. He told us that it sounded like my water had broken and asked us to go to the hospital.”
What happened next?
“We called a friend who came and looked after our sleeping 3-year old son. When we arrived at the hospital, we were taken to an exam room. The doctor did an internal scan. He told us that both the children’s hearts were beating. They were both alive and lively. He told us that my cervix was long, thick and closed. I exhaled and told him that it was great. I continued crying, but it was tears of joy. I was relieved. I remember that the children’s father and I looked at each other and smiled. I thought that everything was well and that we were going home.”
Weren’t you going home?
“I was asked to sit in a chair next to the doctor. He was typing on his computer and a nurse came and asked for my arm. I was a bit baffled. I asked her why she needed my arm? She looked at the doctor and then told me that I was about to be admitted to hospital. She needed to put on an ID wristband. The children’s father asked why. Why couldn’t I just go home and rest? The doctor looked at us and told us that I would go into labor within the next couple of days. My world came tearing down. I started crying again and my children’s father asked bewildered what that meant.”
What were you told?
“We were told that due to a tear in Felix’s – twin B’s – amniotic sac, I’d give birth to two non-viable children. It was a really hard message to receive. The children’s father had to go home to be with our son and I was left at the hospital in a state of shock. When I look back, I have this image of myself as a beggar. Whenever the staff entered my room at the hospital, I would reach out my hands and beg them to help me. I begged them to give me hope. They told me that my odds unfortunately were poor and they had to be realistic. Due to the tear in Felix’s amniotic sac, my cervix would most likely shorten and open and I’d go into labor. I was admitted to hospital on December 20, 2012.”
Could you do anything to comfort yourself?
“I called my dad, who was at his holiday home in Spain at the time. He told me that he’d come home immediately. I told him to wait, there was nothing he could do. We talked on the phone daily. I didn’t do much, but cry, I’m amazed at how many tears I could produce. On December 24 I asked if I could go home for the night. The hospital staff let me, partly because I insisted to, but also because I hadn’t gone into labor yet. They had anticipated that I’d go into labor within 2-3 days after my water broke, but I didn’t.”
How did you feel?
“On Christmas Eve I layed on a couch, watching my family eat and celebrate. I felt like I was on the sidelines. On Christmas Day, early in the morning, I went back to the hospital. During the following days at the hospital, I felt my babies kick for the first time. That was awful. The pregnancy felt more real and it was terrible knowing that I was going to lose them. Then I started getting contractions. I talked with an obstetrician who gave me a pill to stop the contractions. The pill worked, but I had to remain at the hospital. I felt exhausted, I couldn’t accommodate anything. The staff always closed the door behind them when leaving my room and I didn’t like that. It was a dark room and I felt like the white walls were closing in on me. I felt like I was going crazy. I was admitted to a ward where women, who are pregnant less than 24 weeks, are admitted. There were also quite a few women with cancer admitted and several of them died. It was tough to meet family members who were crying in the hallway.”
How did you cope?
“One day I talked to my father on the phone and broke down completely. He booked a flight home and went directly to the hospital. He talked to the staff and told them that he couldn’t recognize me. He asked them if it was possible for me to see a psychologist, but they didn’t have one employed. They told us that I could see the hospital priest, but I didn’t want to. We ended up agreeing that I could go home if I remained on bed rest.”
How closely were you monitored?
“I went to the hospital three times a week for scans. They also did blood tests due to the increased risk of infection.* The children’s father and I weren’t allowed to have sex, not even using protection. During my bed rest, family and friends came by and cleaned, cooked and picked up our son in daycare.”
*A tear in the amniotic sac provides a path for bacteria to enter the womb and puts both the mother and baby at risk of life-threatening infection.
Did you feel optimistic that your children would survive?
“No. However, after a couple of weeks at the hospital I spoke with an elderly doctor who ignited a bit of hope. He saw me crying and asked what was wrong. I told him that I was very scared and I felt that nobody wanted to offer me hope. The hospital staff seemed so pessimistic. He told me, that “as long as there’s life, there’s hope.” It just took those words in order for me to feel more hopeful. We actually changed our daughter’s name after that encounter. We had decided that her name was Ida, but we changed it to Liv.* She was twin A and she was blocking Felix’s way out of my womb. Our first real milestone was week 24. I knew that the hospital staff would do what they could to save the babies if we made it to that week.”
*Liv means life in Danish
How were the babies doing?
“Throughout my pregnancy, the amniotic fluid kept gushing out of me. Nevertheless, at every scan the children seemed to be doing fine.* They were growing as expected. Even though Felix had less amniotic fluid than Liv, he could still move freely. I didn’t think much about whether the children would be born damaged in some way. I worried much more about them not surviving.”
*Low levels of amniotic fluid around a baby increases the risk of umbilical cord compression and can interfere with lung and body formation in early pregnancy.
How was your third trimester?
“I kept being monitored closely. I was at the hospital more than the scheduled three times a week, because I was bleeding from time to time. When I was 33 weeks pregnant* my best friend threw me a baby shower. I had been on bed rest until then, with a few exceptions, where I’d been on minor outings. The baby shower lasted for much of the day. The following day, amniotic fluid gushed out of me more heavily than ever before. I called the hospital and they told me to pack a back. They let me know that I wouldn’t be going home again until I’d given birth. I felt good about it, I knew that my children were mature enough to survive at this point.”
*This is when you’re between 32+0 and 32+6 weeks pregnant.
What happened at the hospital?
“I was given medicine to speed up the babies lung development. After 2-3 days I was told that they would induce labor soon. I was told that Liv was in the standard head first position, but that Felix was breech. I really wanted to give birth vaginally and I was allowed to, but I chose a c-section. I was so afraid that one of the babies would get stuck. I was afraid of not being able to give birth to them, that they wouldn’t get enough oxygen and that the umbilical cords would be around their necks. If Felix had been in a head first position, I think I would have chosen a vaginal delivery. I don’t like needles and I didn’t like the thought of a doctor cutting in me.”
How did the c-section progress?
“I cried all the way through. I began crying, when I put on the hospital clothes. I wasn’t worried about the babies at this point, I was just very scared about the needles and the procedure. I was terrified. It went well, however, and the children were born 12. april 2013 at 33+2 weeks. They were perfect and quite large. They weighed 2440 (5lb, 6oz) and 2420 (5lb, 5oz) grams respectively. They measured around 49 centimetres (19.29 in).”
How did the first few weeks progress?
“The children had very few difficulties due to being born preterm. Both children needed CPAP* treatment, but beyond that they were strong. Part of the staff referred to them as “the miracle twins.” They were in the Neonatal Intensive Care Unit (NICU) for five weeks. Time went by so slowly. It was the longest five weeks of my life. We weren’t allowed to use our cell phones and family members couldn’t visit us in the beginning. During those five weeks, I went outside three times. I felt very isolated, light-headed. The children were sleeping all the time. I missed my eldest son more than anyone. I felt like I was letting him down all the time. When I was on bed rest, we told him that his little brother was sick and that was why I couldn’t be active with him. He didn’t really understand. He wanted me to tuck him in and wanted me to be the one to pick him up from daycare. I felt terrible, that I wasn’t able to. If I had a day or two, where I didn’t leak amniotic fluid, I thought that “now I need to do more for him.” However, there was always that fear inside of me. I felt very ambivalent, I wanted to take care of my eldest son, but I didn’t want to risk the life of my babies.”
*Continuous positive airway pressure (CPAP) is a treatment that uses mild air pressure to keep the airways open.
How did your son react when meeting his siblings?
“He wouldn’t visit us for the first two weeks. We had tried to explain to him why I had to be admitted for several weeks and that didn’t go very well. We found out that he was under the impression that all doctors walk around and cut bellies open at the hospital. Nevertheless, it was a very happy reunion, when he finally did visit. He was so proud. He was standing on a small stool, looking at his siblings. He kept saying “this is my little sister” and “that is my little brother.” It was so nice to have him there.”
How did feeding the babies go?
“In the beginning they eat through a tube. After a while I tried tandem nursing, but I couldn’t manage it. When I had gotten one child up and reached for the other, the first one would latch off. The staff suggested that I nursed one baby, while I simultaneously fed the other one a bottle. That worked well. I would swop, so both were breastfed every other time. Then – from one day to the next – we were told that we could go home. After returning home, I didn’t nurse for long. Our daughter didn’t want to nurse, she preferred the bottle. Also, I wanted their father to be able to help and I wanted to be more around our eldest son.”
Looking back, what was hardest during the weeks in NICU?
“The uncertainty, the unclear answers and missing my elder son. I missed him desperately, I was longing for him. I remember my mother telling me during my pregnancy with him, that I’d love him from the first moment I laid eyes on him. I didn’t when he was newborn. I thought that he was wonderful and I knew that I’d protect him, but I didn’t love him until I knew him better. I felt the same way with the little ones. I didn’t know them yet.”
How did the first weeks at home go?
“I’ve never felt that it’s hard being a mother of twins. It was harder for me becoming a mom the first time around. When I didn’t have any children, I was used to being 100 percent independent and had to learn to deal with being more restrained. When I had the twins, I had dealt with those issues. Also, I succeeded early on at synchronizing them, so they eat and slept at the same time. Nevertheless, we did experience other problems. My son developed colic, and I sometimes felt I was missing a couple of extra arms. I felt guilty that I couldn’t be there 100 percent, especially for my daughter.”
How did you cope with the feelings of guilt?
“I thought about the fact that my daughter is different from her brother. Liv didn’t crave the same amount of physical contact. Liv would normally lie next to me – instead of on my chest like Felix – and that enabled us to have a lot of eye contact. I was looking at her a lot, cuddling her. In general I tell myself that I’m doing the best that I can. I’m not an octopus. I look at my children and think about how they seem. Are they thriving? If they are, then what’s the big deal if one of them has to wait a bit getting fed? It’s the same about feeling guilty choosing not to breastfeed. I remind myself that love comes from the heart, not my breasts.”
When did they sleep through the night?
“They’ve generally been good at sleeping and they still are. When they were about 1 year old, they slept from evening until the next morning without being fed. In the first few months at home, I slept with Felix on my chest. I teached myself to fall asleep that way, because nothing else worked.”
Any advice for future twin parents?
“Twins or not, you need to have a strong relationship as parents. The children’s father and I didn’t and we split up when the babies were six months old. I think it sometimes affect people differently when they become parents and that can make you grow apart.”
Would you like to share your twin birth story with the readers of this site? Please write us an e-mail. We would love to publish your story. Twin birth stories will continually be published on this site.







Twin birth stories – c-section & natural birth
Some women attempt giving birth to twins naturally and end up with a c-section for one or both of their twins. That doesn’t necessarily mean that they had a bad twin birth experience. It depends very much on how their birth progressed and on how well they connected and cooperated with the people present at the delivery.
Positive twin birth stories: Merian’s twin birth story
Mother: Merian Desireé Brastrup Clasen
Children: Older sister Mynte (born 2006) and fraternal twin girls Merle and Nælde (born 2009 in Denmark) younger sister Cirkel (born 2010).

When did you go into labor?
The labor was induced, when I was 37+4 weeks pregnant. At about 8.30 AM the midwife did a premature rupture of membranes – breaking my water. Both children’s heartbeats were monitored via CTG, as we were waiting for contractions. We talked about different kinds of pain relief, especially an epidural. It was my impression that an epidural is more or less standard procedure during a twin birth, so it can be used at a potential c-section.
What did you choose?
Prior to giving birth to my twins, I had an easy delivery with my firstborn, and I wasn’t especially interested in getting an epidural. My midwife talked to the midwife in charge, and they agreed that it wasn’t necessary for me to get an epidural up front, as I had gone through a vaginal birth before. Also, both twins were facing head down. It seemed like it would be a straightforward twin birth.
How did the labor progress?
An hour after inducing labor, nothing had happened. Then I got an intravenous drip to stimulate contractions and quickly got frequent contractions. After one and a half hour I had a vaginal exam. I was 4-5 centimeters dilated. I remember my husband talking to the midwife about me being about halfway through labor, and I, myself, thought that I had a couple of hours left. However, after about 15 minutes I felt a downward, heavy sensation. I thought something was wrong with the contractions. When I told the midwife about this, suddenly she got very busy. She accidentally dropped the equipment, she had just found, on the floor. At that point she and a medical student were the only ones present.
What happend next?
Hastily the 8-10 persons, who should participate in the delivery of the babies, were summoned. At about 1.30 pm - after a couple of labor contractions – twin A was born. This occurred around 2 hours after the drip, that stimulated contractions, was turned on. Twin A had a brief exam and was passed over to her father. During this phase twin B was closely monitored by CTG and scanner. The membranes were punctuated and I felt a heavy shower. Trouble presented itself, when they wanted to put an electrode on the baby’s head. It wasn’t the baby’s head they could feel.
How did they proceed?
They scanned over and over again and another midwife and doctor was called to the delivery room. After a bit of time one of the midwives succeeded in placing the electrode on the baby’s head. 2-3 different persons felt internally as they were scanning. After a while they agreed that they could feel an elbow or shoulder, and the doctor decided that a c-section was necessary. This was partly because the baby’s heartbeat was a bit affected. I went to the operating room and at 14.21 pm – 50 minutes after her sister – twin B was born at an emergency c-section. Twin B was examined and handed over to her father and newborn sister. After the c-section, I went to recovery, and after a while my husband came with the children, so I was finally able to see them.
How big were the babies?
Merle weighed 2816 grams (6 lb, 3 oz) and measured 49 centimetres (19.29 in). Nælde weighed 2645 grams (5 lb, 13 oz) and measured 50 centimetres (19.69 in). Their weights surprised me. At my last scan during pregnancy, Merle was assessed to weigh about 500 grams (1 lb, 1 oz) less than Nælde. I was concerned about this, worrying about whether or not she was getting enough nourishment. In general, I worried more during this pregnancy than during the pregnancies with my other children.
How were the babies doing?
We were at the hospital for nine days. Merle had infant jaundice and Nælde looked quite yellowish, so they were both placed in light therapy, when they were a few days old. We had problems getting them to gain weight, so they got a milk supplement, with milk I had milked out, after I’d nursed. The time at the hospital was rough, so we were happy the day we were allowed to go home. Not the least to see our oldest daughter, who had been looking forward to getting me back home.
How did the following days progress?
After we returned home we had to go back to the hospital every 48 hours. Hospital staff weighed the babies to ensure that they were gaining sufficient weight. For the first few weeks we had to wake up the children every three hours, around the clock, to feed them.
Overall, both the vaginal birth and the c-section was a good experience. I had quite a lot of pain in the cesarean incision the first few days, but after about 2 weeks I didn’t feel any pain, nor vaginal. I’d say that the twin birth is the easiest birth I’ve been through, at least the birth of Merle (twin A).
Any advice for future twin parents?
There are many different ways of doing things, I don’t know if I have any advice that’s applicable. I think it helps if you are good at relinquishing control. I come from a large family – I have 5 siblings – and I’ve been used to having younger siblings around.
You need to have faith in the fact that you’ll figure out how to handle two screaming children in public - otherwise you won’t get out much. Also, I experienced the first six months with twins as being the hardest. When they were able to do a little bit by themselves, it got easier. In any case, I got two fantastic children out of it, and my, it’s just really special to be a parent of twins. It’s just so great to experience them together.
Would you like to share your twin birth and pregnancy story with the readers of this site? Please write an e-mail to kate@about-twins.com. We would love to publish your account. Twin birth and pregnancy stories will continually be published on this site.




Looking for twin birth stories from mothers who were diagnosed with Twin to Twin Transfusion Syndrome (TTTS) or Twin Anemia Polycythemia Sequence (TAPS) during their pregnancies? Please visit our TTTS and TAPS stories.














